Clinica Chimica Acta:全面的免疫复合物分析可检测源自不育男性和女性的精浆和卵泡液中的疾病特异性免疫复合物抗原
2019-10-17 gladiator MedSci原创
自身免疫性反应和后续的炎症可能是精原性功能障碍和子宫内膜异位症相关不孕的病因。
自身免疫性反应和后续的炎症可能是精原性功能障碍和子宫内膜异位症相关不孕的病因。本研究的目的是在精浆(SP)和卵泡液(FF)的免疫复合物(ICs)中鉴定疾病特异性抗原。
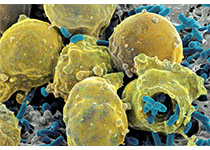
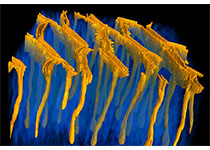
采用纳米液相色谱-串联质谱联用技术,对不育夫妇辅助生殖标本进行免疫复合体分析,综合鉴定生物体液中集成到ICs中的抗原。42名男性患者,包括少精症(n = 6),弱精子症(n = 8)和精液分析正常患者(n = 28)。58名女性患者,包括卵巢子宫内膜异位症患者(n = 10)和无疾病对照女性(n = 48)。
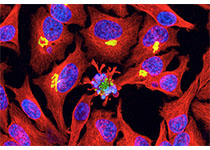
研究在少精子症患者中发现了4种疾病特异性抗原,而在弱精子症患者中发现了5种疾病特异性抗原,其中一些抗原参与了精子发生。仅在子宫内膜异位症患者中检测到8种抗原。
研究发现了与男性和女性不育的发病机制相对应疾病特异性抗原的功能特征。ICs的形成可能通过相关蛋白功能的丧失而导致精原性功能障碍和子宫内膜异位症相关不孕。免疫复合物分析有望成为研究不孕症新诊断方法和治疗策略的一个有价值的工具。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#卵泡#
41
#复合物#
37
#CTA#
24
#特异性#
22
#免疫复合物#
44
#抗原#
0