Nat Med:Axicabtagene ciloleucel作为高危大B细胞淋巴瘤的一线治疗
2022-03-23 MedSci原创 MedSci原创
Axi-Cel作为高风险LBCL患者一线治疗的非常有效,并且具有可控的安全性。
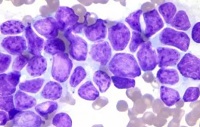
大B细胞淋巴瘤(LBCL)占全球非霍奇金淋巴瘤所有新诊断的40%左右,使其成为最常见的亚型。约60%的LBCL患者对标准一线化学免疫治疗方案有持久反应,例如6个周期的利妥昔单抗、环磷酰胺、多柔比星、长春新碱和强的松(R-CHOP)或剂量调整的依托泊苷、强的松、长春新碱、环磷酰胺、多柔比星和利妥昔单抗(DA-EPOCH-R)。采用标准一线化学免疫疗法治疗的高危LBCL患者的结局较差。

近日,顶级医学期刊Nature Medicine上发表了一篇研究文章,在这项2期、多中心、单组ZUMA-12研究(Clinical Trials.gov NCT03761056)中,研究人员评估了滤泡性淋巴瘤CAR-T细胞疗法Axicabtagene Ciloleucel(Axi-Cel),一种自体抗CD19嵌合抗原受体(CAR)T细胞疗法,对40名 高危LBCL患者一线疗法的效果。

该试验的主要结局是完全缓解率(CRR),次要结局是客观缓解率(ORR)、缓解持续时间(DOR)、无事件生存期(EFS)、无进展生存期(PFS)、总生存期(OS)、安全性评估、中枢神经系统(CNS)复发、血液中CART 细胞和细胞因子水平。

可评估疗效患者(n = 37)的主要终点得到了满足,CRR为78%(95%置信区间(CI)为62-90),ORR为89%(95%CI为75-97)。截至2021年5月17日(中位随访时间为15.9个月),73%的患者保持客观缓解;未达到中位DOR、EFS和PFS。分别有3名患者(8%)和9名患者(23%)发生 3级以上细胞因子释放综合征(CRS)和神经系统事件。没有患者发生与治疗相关的 5级事件。所有患者均出现强劲的CART细胞扩增,达到峰值的中位时间为8 天。
由此可见,Axi-Cel作为高风险LBCL患者一线治疗的非常有效,并且具有可控的安全性。
原始出处:
Sattva S. Neelapu,et al.Axicabtagene ciloleucel as first-line therapy in high-risk large B-cell lymphoma: the phase 2 ZUMA-12 trial.Nature Medicine.2022.https://www.nature.com/articles/s41591-022-01731-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Gene#
46
#Nat#
35
#CEL#
29
#细胞淋巴瘤#
27
学习了。
54
#B细胞#
33
#Med#
27