Cancers:黏液性结直肠腺癌无远处转移患者中辅助化疗的预后价值
2022-03-11 yd2015 MedSci原创
研究表明,黏液性腺癌(MAC)患者的预后较腺癌(AC)患者的更差,尤其是在III期患者中,辅助化疗也不能显著改善患者预后。
在结直肠癌中,黏液性腺癌(MAC)患者的预后较腺癌(AC)患者的要差。但是粘液性腺癌(MAC)的预后指标仍存在争议。因此,来自韩国的团队开展了相关研究,评估黏液性腺癌无远处转移患者的预后因素以及辅助化疗在该类患者中的作用。相关结果发表在Cancers杂志上。
研究纳入22,779名患者,其中AC和MAC组分别有22050例(96.8%)和729例(3.2%)患者。中位随访时间为54.5个月。
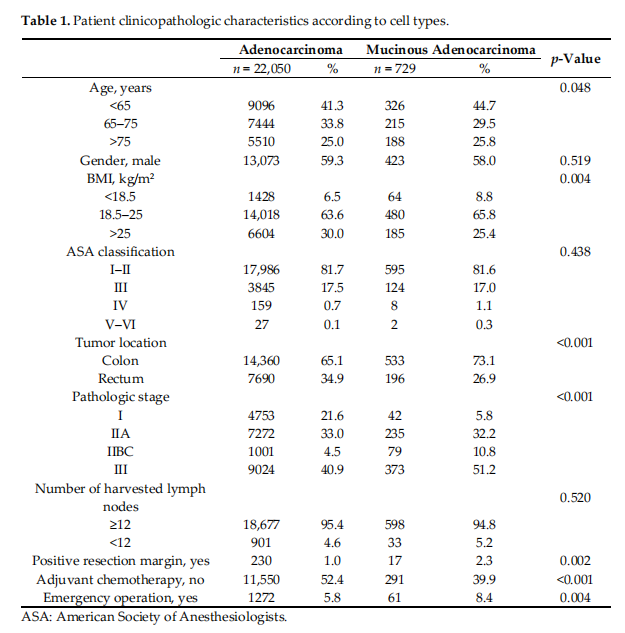
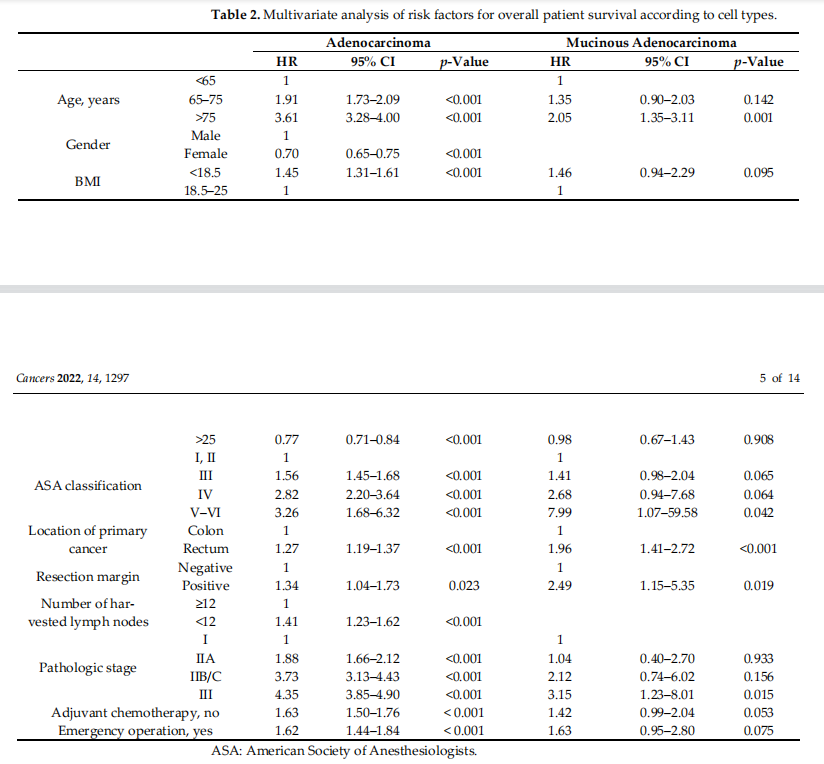
多因素预后分析发现,两组的危险因素类似。然而,低、高BMI是AC的显著危险因素,但在MAC中无统计学差异。此外,HR在AC组中按分期是逐步增高,而在MAC中没有。MAC组中,病理III期组差异有统计学意义,但在病理型IIA和IIB/C肿瘤没有差异。MAC组未接受辅助化疗的HR (HR = 1.42)低于AC组(HR = 1.63)(p = 0.053)。
MAC组患者的OS较AC组患者差(5年OS率: 79.4 vs. 70.0%,p<0.001);I期、IIA期、IIB/C期患者OS在两组间无显著差异。然而,III期患者中MAC组的OS低于AC组(5年OS率: 71.8 vs. 61.6%,p<0.001);在亚组分析中,接受辅助化疗的AC和MAC组患者比未接受辅助化疗的患者有更好的生存期,这一结果在II期和III期是一致的。在IIA期和IIB/C期,MAC辅助化疗患者的OS与AC辅助化疗患者的OS相似。然而,在病理III期,尽管给予辅助化疗,MAC患者的OS仍低于AC患者(5年OS率: 78: 67.2%, p<0.001)。
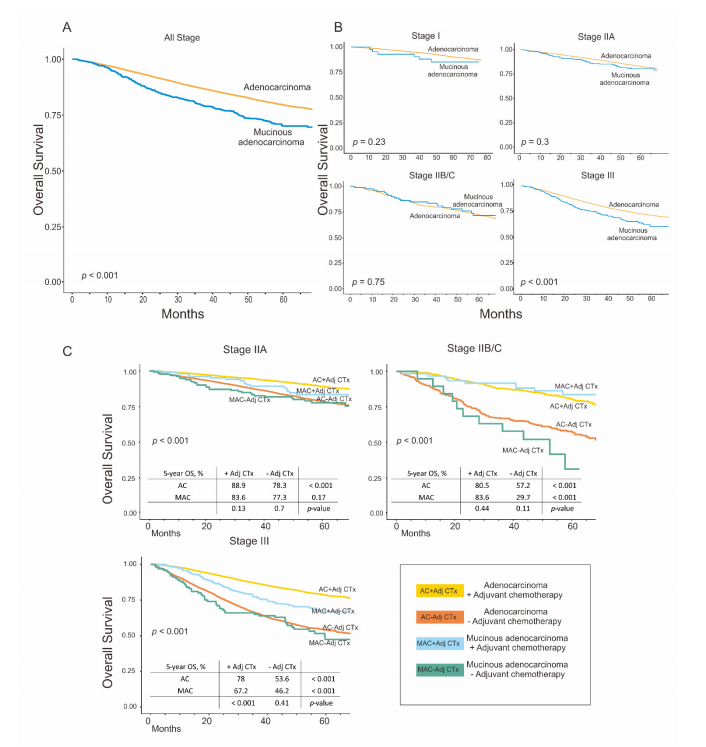
使用倾向性匹配评分后,两组的OS跟初始分析的较为一致。

综上,研究表明,黏液性腺癌(MAC)患者的预后较腺癌(AC)患者的更差,尤其是在III期患者中,辅助化疗也不能显著改善患者预后。
原始出处:
Bong JW, Gim JA, Ju Y, Cheong C, Lee SI, Oh SC, Min BW, Kang S. Prognosis and Sensitivity of Adjuvant Chemotherapy in Mucinous Colorectal Adenocarcinoma without Distant Metastasis. Cancers (Basel). 2022 Mar 2;14(5):1297. doi: 10.3390/cancers14051297. PMID: 35267605.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#ERS#
28
#预后价值#
27
#远处转移#
33
#结直肠#
30