NEJM:罗氏旗下基因泰克的类风湿药物Actemra在COVID-19 III期临床试验中未能达到其主要终点
2021-03-16 Oranhgy MedSci原创
类风湿关节炎药物Actemra在COVID-19试验中未能达到其主要终点。
近日,基因泰克报告其类风湿关节炎药物Actemra在COVID-19试验中未能达到其主要终点。同时也报告了Vir和葛兰素史克(GlaxoSmithKline)针对COVID-19的抗体显示出85%的疗效,下一步将申请紧急使用授权(EUA)。

来源:veritatisadvisors
基因泰克公司发表在NEJM上有关严重Covid-19住院患者使用Tocilizumab的研究(COVACTA)显示,其在重症COVID-19患者中开展的Actemra (tocilizumab托西利珠单抗)联合吉利德(Gilead) Veklury (remdesivir) III期临床试验,与安慰剂联合Veklury相比,使用托西利珠单抗在28天时没有显着改善Covid-19住院患者临床状况或降低死亡率,意味着未能达到主要终点。
Actemra是一种人源化白细胞介素6 (IL-6)受体拮抗剂,适用于使用一种或多种抗风湿药物(如甲氨蝶呤)不能完全缓解的中度至重度活动期类风湿性关节炎成人患者。
在这项针对欧洲和北美9个国家(加拿大,丹麦,法国,德国,意大利,荷兰,西班牙,英国和美国)的62家医院进行的试验中。研究人员对经过改良的意向性治疗人群的主要和次要结局进行了疗效评估,其中包括所有接受随机分组并接受一定剂量的托西利珠单抗或安慰剂治疗的患者。
对于本试验中患者的评价,基线定义为第1天给予托西利珠单抗或安慰剂前的最后一次观察。根据以下类别对患者的临床状态进行序数表评估。1、出院或准备出院;2、在非重症监护室(ICU)住院,不补充氧气;3、非ICU住院,补充氧气;4、ICU或非ICU住院,进行无创通气或高流量氧气;5、ICU住院,插管和机械通气;6、ICU住院,体外膜氧合或机械通气和额外器官支持;7、死亡。在基线和住院期间每天记录临床状态。
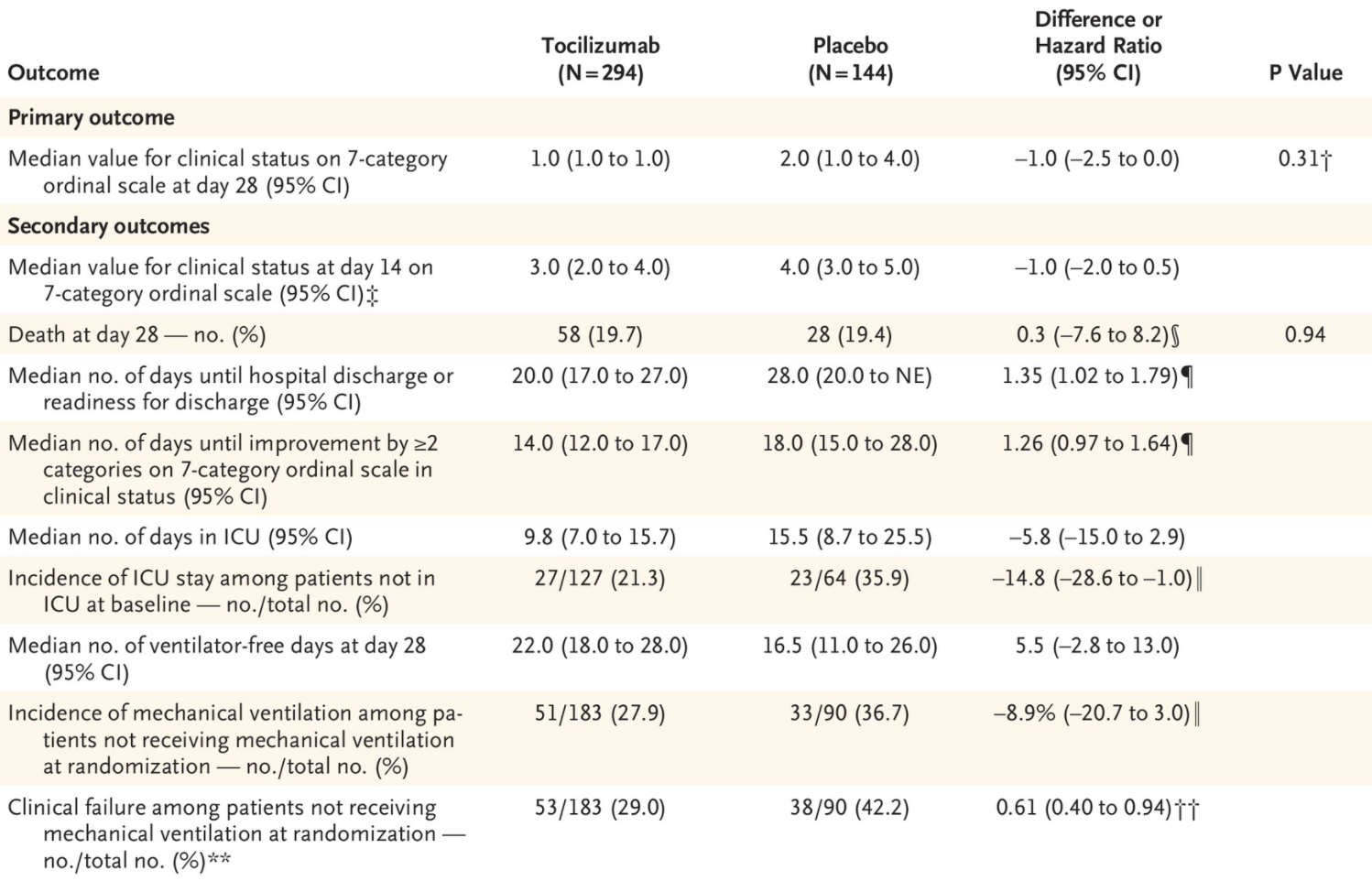
主要疗效结果是第28天的临床状态,用七类序数表评估。关键的次要疗效结果是序数表上第14天的临床状态、第28天的死亡率、第28天无呼吸机天数、序数表上从基线改善至少两个类别的时间,以及出院或准备出院的时间;后者被定义为在呼吸环境空气或2升或更少的补充氧气时,体温和呼吸频率正常,氧饱和度稳定。其他次要结果是直到临床失败的时间,其定义为死亡、住院期间停止参与试验、启动机械通气或ICU转移或基线时正在接受机械通气或在ICU的患者中临床状态恶化1类;随机时未接受机械通气的患者中启动机械通气的情况;基线时未在ICU的患者中ICU转移的发生率;以及ICU住院时间。
主要与次要结果

临床状况和出院情况的变化
分析结果显示,在452名接受随机化的患者中,438名(托西利珠单抗组294名,安慰剂组144名)被纳入一级和二级分析。在第28天,托西利珠单抗组的序贯量表临床状态的中位值为1.0(95%置信区间[CI],1.0~1.0),安慰剂组的中位值为2.0(非ICU住院,不补充氧气)(95%CI,1.0~4.0)。
在安全性方面,托西利珠单抗组295例患者中103例(34.9%)和安慰剂组143例患者中55例(38.5%)发生严重不良事件。第28天的死亡率,托西利珠单抗组为19.7%,安慰剂组为19.4%(95%CI,-7.6~8.2;名义P=0.94)。

archive.fortune.
考虑到COVID-19对全球的影响。鉴于此结果,基因泰克首席医疗官兼全球产品开发主管Levi Garraway表示,对研究未能达到其终点感到失望。除此之外,仍然认为,总体数据表明,托西利珠单抗在治疗某些COVID-19患者方面具有潜在作用,接下来也将进一步与卫生当局讨论结果。
基因泰克目前仍在评估REMDACTA、COVACTA和EMPACTA试验的数据,以及Actemra治疗COVID-19肺炎的其他研究。
原文出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#主要终点#
32
#III#
25
#I期临床试验#
25
#I期临床#
29
#EMR#
35
#II期临床试验#
26
#类风湿#
28
#II期临床#
29
#Actemra#
34
#III期临床试验#
39