BMJ子刊:1型糖尿病患者动脉硬化的预测因素有哪些?性别优势体现出来了?
2022-01-18 MedSci原创 MedSci原创
在青少年和成人中,只有年龄、性别和FMD与动脉硬化程度相关。与男性相比,女性动脉僵硬程度较低,且具有类似的一氧化氮依赖性内皮功能。
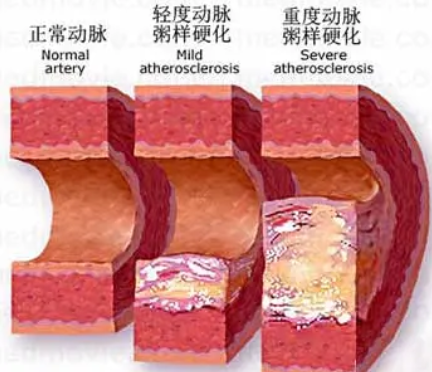
随着年龄的增长和其他心血管危险因素的增加,人体的大弹性动脉会逐渐变硬,这一过程对心血管系统和人体的主要器官产生了许多有害后果,因为动脉硬化程度是心血管疾病 (CVD) 的独立风险决定因素。糖尿病 (DM) 是与动脉硬化密切相关的心血管危险因素,本研究的目的是确定哪些血流动力学和人口统计学因素可以预测该人群的动脉硬化。
研究组对 41 名无微血管并发症的1型糖尿病成人和青少年进行了颈-股动脉脉搏波速度(cfPWV)检查。进行了两个普通最小二乘回归分析以确定cfPWV与年龄、糖尿病病程、性别和血红蛋白A1c的相关性,以及其与增强指数 (AIx)、平均动脉压、血流介导的血管扩张功能(FMD) 和心率之间的关系。
结果显示,年龄、性别和FMD为这些1型糖尿病患者提供了有关cfPWV的独特预测信息。尽管心血管危险因素相似,但男性的cfPWV高于女性,在其他大血管结果(包括FMD和AIx)方面没有观察到差异。
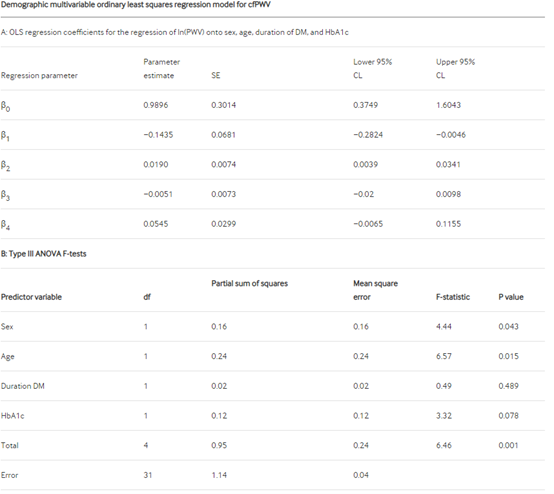
cfPWV的人口统计学多变量普通最小二乘回归模型:性别和年龄提供了有关cfPWV的独特预测信息,而DM持续时间和HbA1c则没有。所有四个变量作为一个整体提供了有关cfPWV的重要预测信息。
总而言之,在青少年和成人中,只有年龄、性别和FMD与动脉硬化程度相关。与男性相比,女性动脉僵硬程度较低,且具有类似的一氧化氮依赖性内皮功能。有必要进行更大规模的前瞻性研究,以确定1型糖尿病患者动脉功能障碍的时间顺序和性别差异。
参考文献:Love KM, Horton WB, Patrie JT, et al Predictors of arterial stiffness in adolescents and adults with type 1 diabetes: a cross-sectional study BMJ Open Diabetes Research and Care 2022;10:e002491. doi: 10.1136/bmjdrc-2021-002491
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#BMJ#
43
#1型糖尿病患者#
41
学习每日都有提高
54
#预测因素#
39
#糖尿病患者#
34