TCT 2020|VOYAGER PAD研究:药物涂层装置在外周动脉血运重建中长期安全性得到认可
2020-12-30 门诊新视野 《门诊》杂志
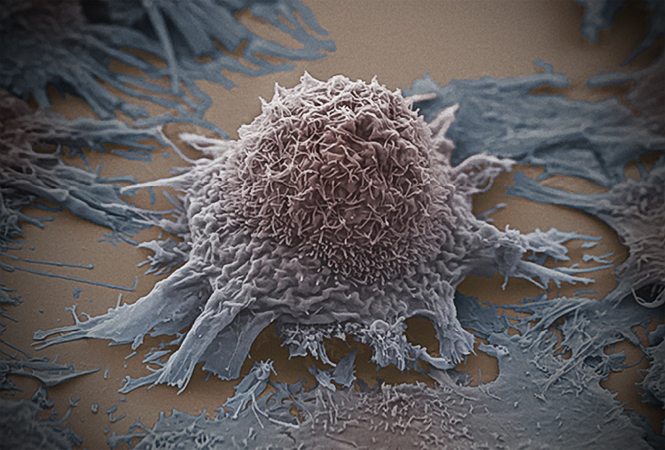
认可 对于有症状的外周动脉疾病(PAD)患者,腔内血运重建可有效改善症状及保肢率,但存在术后再狭窄的困扰。紫杉醇药物涂层装置(DCB)的设计初衷就是为了解决再狭窄问题以及改善通畅率。
认可 对于有症状的外周动脉疾病(PAD)患者,腔内血运重建可有效改善症状及保肢率,但存在术后再狭窄的困扰。紫杉醇药物涂层装置(DCB)的设计初衷就是为了解决再狭窄问题以及改善通畅率。而Katsanos教授提出DCB的使用与长期死亡率增加有关,但其关键研究5年随访数据存在14%~38%的失访率。为探究紫杉醇药物装置与全因死亡率的关系,并评估利伐沙班2.5 mg每天两次+低剂量阿司匹林vs. 单用低剂量阿司匹林对主要疗效终点的影响是否与不用DCB一致,Connie N. Hess教授代表团队开展了相关研究,并于当地时间2020年10月18日,在第三十二届美国经导管心血管治疗学术会议虚拟会议(TCT CONNECT)LBCT专场上发表结果。
研究方法
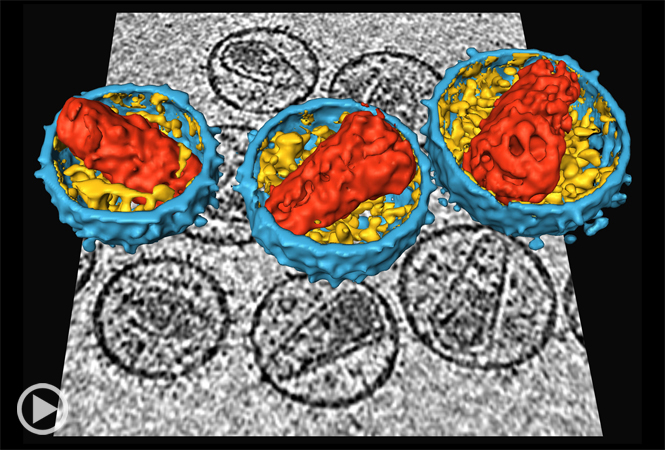
VOYAGER PAD研究是一项随机、双盲、对照研究。对于6,564名接受外周动脉血运重建的有症状PAD患,随机分配至利伐沙班组(2.5 mg每日两次,n=3,286)和安慰剂组(n=3,278),并根据血运重建方式(外科手术组或腔内治疗组)以及是否使用氯吡格雷进行分层。中位随访时间为28个月,主要终点为DCB vs. 非DCB全因死亡率,以及利伐沙班组vs. 安慰剂组的急性肢体缺血、血管疾病引起的大截肢、心梗、缺血性卒中或心血管死亡(图1)。
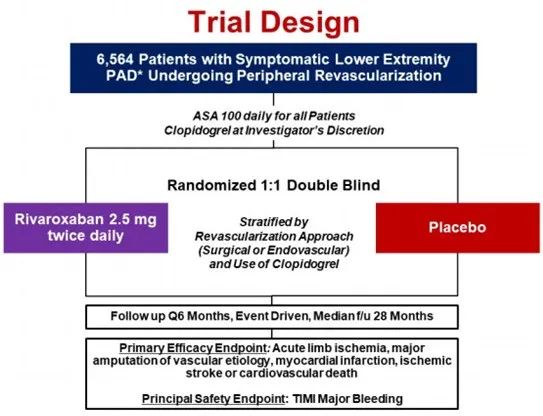
图1. 研究设计流程图
研究结果
6,564例患者中,接受腔内治疗的有4,379例(67%,包括杂交手术)。其中,3,021(69%)例使用DCB,1,358(31%)例不使用DCB。使用DCB的患者中,1058(78%)例使用药物涂层球囊,235(17%)例使用药物洗脱支架,剩下的70(5%)例患者两者都使用。中位随访时间31个月(IQR 25~37),99.6%的患者明确生命体征。
研究结果显示,全因死亡率非DCB组vs. DCB组为12.6% vs. 12.1%(HR 0.95,95%CI 0.83~1.09,P=0.49)(图2)。对混杂因素进行调整,并未发现死亡率与DCB的相关性。无论是否使用DCB,有症状的PAD血运重建后,利伐沙班2.5 mg每天两次+阿司匹林 vs. 单用阿司匹林在减低缺血肢体和心血管事件获益上一致,总HR为0.85,95%CI 0.76~0.96,P=0.0085(图3)。
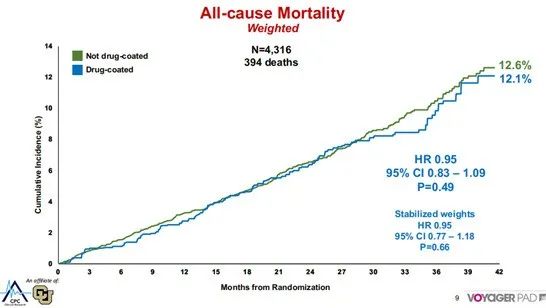
图2. 全因死亡率
图3. 根据是否使用DCB,判断利伐沙班的效果
总 结
VOYAGER PAD研究作为一项大样本量(n=4,316)研究,长期随访结果显示紫杉醇DCB的使用与死亡率无关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#动脉血#
39
#GER#
37
#长期安全性#
57
#TCT#
0
#外周动脉#
33