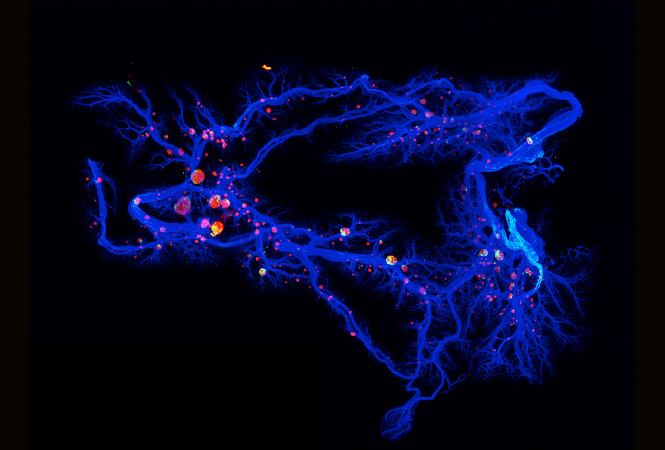
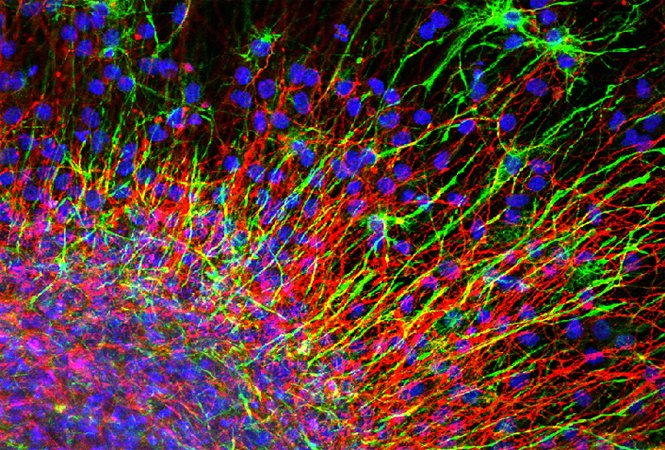
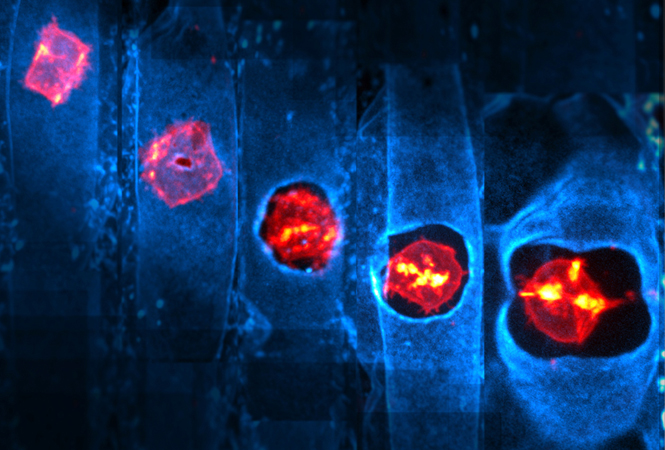
肺动脉高压(PAH)是一种衰弱性疾病,与肺动脉远端血管重塑有关,导致肺动脉压力升高、右心室肥大和死亡。虽然呈现出高水平的DNA损伤,通常会危及其生存能力,但肺动脉平滑肌细胞(PASMCs)从PAH患者的肺动脉平滑肌细胞(PASMCs)表现出类似癌症的增殖和抗凋亡表型,是导致血管腔湮灭的原因。在癌细胞中,丝氨酸/苏氨酸蛋白激酶CHK1(checkpoint kinase 1)的过量表达被利用来抵消它们所受到的过量的DNA损伤侵袭。本研究旨在确定PAH-PASMCs是否形成了由CHK1介导的协调反应,以克服DNA损伤,使细胞存活和增殖。结果显示,与对照组相比,CHK1的表达在分离的PASMCs和PAH患者的远端PAs中明显增加,并且在多个辅助动物模型中重述了该疾病,包括单核细胞移植大鼠和猿猴免疫缺陷病毒感染的猕猴。使用药理和分子功能丧失方法,我们发现CHK1促进PAH-PASMCs增殖和抗凋亡。此外,我们发现抑制CHK1会诱导DNA修复蛋白RAD 51的下调和严重的DNA损伤。在体内,我们发现,药理抑制CHK1显著减少血管重塑,改善了2个实验性大鼠模型的PAH的血流动力学参数。综上所述,该研究结果表明,CHK1通过减轻DNA损伤在PAH-PASMC中发挥促增殖作用,提示CHK1抑制可能是PAH患者有吸引力的治疗选择。
【2】射血分数保留和肺动脉高压的心衰患者弥漫性右心室纤维化情况
右心室(RV)功能障碍与合并病性肺动脉高压和伴有射血分数(PH-HFpEF)保留的心力衰竭不良预后有关,但尚不清楚导致RV功能障碍的机制。我们评估了PH-HFpEF中弥漫性RV心肌纤维化的程度和临床相关性,结果显示,与PAH相比,PH-HFpEF的患者年龄更大,高血压和阻塞性睡眠呼吸暂停的发生率更高。虽然PH-HFpEF和PAH之间的RV ECV相似,但与PAH相比,PH-HFpEF的总肺阻力较低。PH-HFpEF中的RV ECV与较差的RV结构和RV功能的指标较差有关,但与RV后负荷无关。相反,PAH中的RV ECV与RV后负荷之间有很强的相关性。综上所述,该研究结果表明,正如ECV检测的结果一样,PH-HFpEF中存在弥漫性房室纤维化,与不良的房室结构和功能重塑有关,但与肺血管病变程度无关。在PH-HFpEF中,弥漫性RV纤维化的发生可能与RV后负荷程度不相称。
【3】法舒地尔可以改善CHD-PAH患者的血流动力学,特别是60-mg剂量
在伴有严重肺动脉高压(CHD-PAH)的先天性心脏病患者中,法舒地尔的最佳剂量仍有争议。本研究旨在对比伴重症肺动脉高压的先天性心脏病成人患者中不同剂量的法舒地尔治疗后的急性血流动力学变化。纳入60例CHD-PAH的成人患者,将其随机分配到法舒地尔30或60毫克。通过右心导管检查,在基线和法舒地尔30分钟后测量血流动力学参数。从肺动脉、右心室、右心房、右心房、上腔静脉和下腔静脉、股动脉获得血气结果。计算了肺血管阻力(PVR)和全身动脉阻力(SVR)。结果显示,sPAP、平均PAP以及PVR在60-mg组中比30-mg组更明显。所有患者均无明显的与外周血压相关的不良反应。总之,该研究结果表明,法舒地尔可以改善CHD-PAH患者的血流动力学,特别是60-mg剂量,可以改善患者的血流动力学,没有出现严重的不良反应。
【4】自动正向气道压治疗可降低急性心力衰竭合并肺动脉高压和阻塞性睡眠呼吸暂停患者的肺部压力
肺动脉高压(PH)在急性失代偿性心力衰竭(ADHF)患者中极为常见,并预示着死亡率的增加。阻塞性睡眠呼吸暂停(OSA)在充血性心力衰竭患者中很常见,可能导致肺动脉高压进一步升高。本研究评估了正气道压(PAP)治疗对ADHF入院的OSA患者的PH的影响。该项两中心随机对照试验,比较了伴有OSA的ADHF的护理标准(SOC)治疗与加用PAP治疗的比较。纳入21名患者,以1:1随机分配至SOC与SOC加48小时PAP治疗方案。在干预臂中,治疗前和48小时PAP治疗后的平均肺动脉收缩压(PASP)差异为-15.8±3.2,而SOC臂的平均PASP差异为-5.2±2.6。此外,干预组的射血分数也有所改善。干预组的三尖瓣环平面收缩压偏移(TAPSE)和右心室收缩面积也有显著改善,但NT-pro-BNP和6分钟步行距离没有改善。总之,该研究结果表明,对于患有ADHF和OSA的患者,在SOC治疗中增加48小时的PAP治疗可显著降低PH。此外,PAP治疗能够改善左右心室功能。
C-X-C趋化因子受体4型(CXCR4)可能参与肺动脉高压(PAH)的发展。据描述,CXCR4抑制剂AMD3100对预防PAH模型中的肺动脉肌化有积极作用。西林素是一种传统药物,对CXCR4有拮抗作用。本研究中,我们利用大鼠PAH模型探究了西林素的作用。结果显示,西林素治疗1周降低RVSP和Fulton指数。治疗2周,可降低RVSP、Fulton指数、%MT和VOS,并可降低肺动脉中CXCR4、SDF-1和TNFα的表达。相比之下,治疗3周未能改善PAH。随着时间的推移,RVSP、Fulton指数、%MT和VOS逐渐增加,而CXCR4和TNFα的表达在PAH发生2周后出现下降。3周后,SDF-1、c-Kit和SCF开始下降,5周后,MCP1和IL-6逐渐积累。总之,CXCR4抑制剂silibininin可能通过抑制CXCR4/SDF-1轴,可以改善PAH的病情,直到PAH成为严重的、不可逆的病症。西林素可降低肺动脉压力,延缓肺动脉闭塞和肺血管重塑。
【6】肺动脉高压患者N端脑钠肽与长期预后的关系
NT-proBNP(N-末端原脑钠肽)水平被纳入PAH指南中的肺动脉高压的多参数风险评估方法中。然而,支持使用NT-proBNP风险阈值评估PAH预后的数据有限。GRIPHON试验为在对照临床试验中评估NT-proBNP阈值的预后价值提供了一个机会,并可根据这些阈值评估对司来帕格的反应。将患者随机分配给司来帕格或安慰剂。结果显示,在这两个阈值的基础上,基线和随访NT-proBNP类别可高度预测未来研究期间的发病率/死亡事件(P<0.0001)。在时间依赖性分析中,与NT-proBNP高水平的患者相比,偏低和中等水平的患者,经司来帕格治疗后发病/死亡事件的风险分别降低了92%和83%,经安慰剂治疗的患者分别降低了90%和56%。在基线和时间相关分析中,司来帕格降低了所有3个NT-proBNP类别的发病/死亡事件的风险,而在中度和低NT-proBNP亚组中,司来帕格的治疗获益更为明显。总之,这些分析进一步确立了NT-proBNP水平在PAH中的预后相关性,并为NT-proBNP水平与治疗反应的关联提供了第一个证据。使用2组类似的阈值,这些分析支持了低、中、高NT-proBNP水平作为欧洲心脏病学会/欧洲呼吸学会管理PAH患者的多参数风险评估方法的一部分的相关性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











好
69
#动脉高压#
0
#研究进展#
38
#PAH#
49
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
63