Front Cardiovasc Med:左心衰竭所致肺动脉高压的患病率和生存率
2022-08-21 刘少飞 MedSci原创
本研究的目的是:(1)描述 LHF 患者 PH 的患病率;(2) 计划和对 PH-LHF 患者进行长期随访,以估计生存率;(3)探讨可能预测PH-LHF死亡的潜在危险因素。
肺动脉高压(PH)已成为一个日益普遍的全球健康问题。据估计,全球约 1% 的人口的患病率在 65 岁以上的个体中增加了高达 10% 。PH 的临床分类分为 5 组,左心衰竭所致 PH(PH-LHF)为第 2 组,定义为毛细血管后 PH [平均肺动脉压 (mPAP) ≥ 25 mmHg 和肺动脉楔压 (PAWP) > 15 mmHg]。由于全球 65 岁以上人口的迅速增加,左心衰竭 (LHF) 的总体发病率正在增加,LHF 正在成为 PH 的主要原因,影响大约 5% 的 65 岁或以上的人.
左心衰竭导致的肺动脉高压是左心室舒张功能障碍性心力衰竭伴射血分数保留 (HFpEF) 或射血分数降低心力衰竭 (HFrEF) 的常见合并症,以往研究报告的患病率范围为 40% 至 75%对于 PH-HFrEF,PH-HFpEF 为 36% 至 83%。然而,这种流行源于黄金诊断标准 (RHC) 的不统一应用。例如,一些报告依赖于通过超声心动图测量的肺动脉收缩压 (PASP) 或使用不同的诊断标准。因此,PH-LHF 的真实患病率尚不清楚。
在过去的二十年里,LHF 患者的死亡率显着下降。然而,近年来 PH-LHF 的死亡率仍然很高。与肺动脉高压 (PAH) 患者相比,PH-LHF 的生存期较差。PAH 有几个实用的风险表,用于对预后进行分层,提供治疗目标和随访策略。然而,PH-LHF 的实用且可靠的风险表不可用。识别潜在的危险因素可能有助于缓解 PH-LHF 患者的高死亡率问题。因此,本研究的目的是:(1)描述 LHF 患者 PH 的患病率;(2) 计划和对 PH-LHF 患者进行长期随访,以估计生存率;(3)探讨可能预测PH-LHF死亡的潜在危险因素。
研究方法:
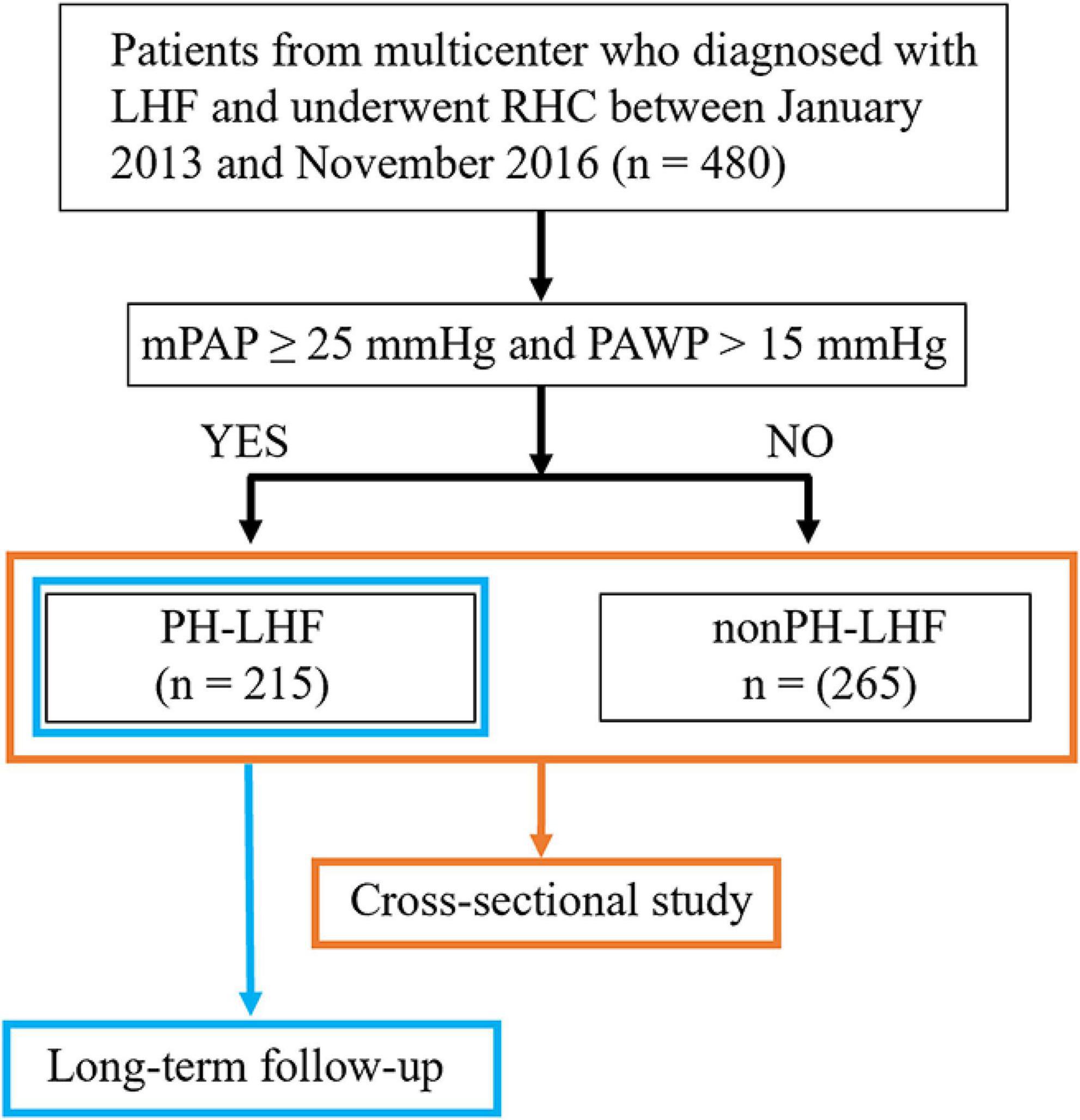
对 2013 年 1 月至 2016 年 11 月期间接受右心导管 (RHC) 的左心衰竭 (LHF) 患者的前瞻性队列研究进行回顾性分析。终点是全因死亡率。每 6 个月 ± 2 周进行一次随访。
研究结果:
共纳入 480 例 LHF 患者,其中 215 例(44.8%)患有 PH-LHF。冠状动脉疾病(CAD)组的 PH-LHF 比例显着低于无 CAD 组(41.3% vs. 57.8%,p = 0.003)。然而,多变量逻辑回归分析显示 CAD 与 PH-LHF 无关(调整后的 OR:1.055,95% CI:0.576 – 1.935,p = 0.862)。215 名 PH-LHF 患者中有 75 名(34.9%)在中位随访 84.6 个月期间死亡。所有 PH-LHF 患者的 1 年、3 年、5 年和 8 年生存率分别为 94.3%、76.9%、65.8% 和 60.2%。在多变量 Cox 分析中,纽约心脏协会功能分级 (NYHA FC)、血红蛋白和肺动脉收缩压 (sPAP) 与 PH-LHF 死亡率相关。
研究结论:
PH 常见于 LHF 患者,患病率约为 45%。PH-LHF 患者的死亡率仍然很高。NYHA FC、血红蛋白和 sPAP 是 PH-LHF 死亡率的独立风险预测因子。这些发现可能对未来临床试验登记中的风险分层有用。
参考文献:
Lin Y, Pang L, Huang S, Shen J, Wu W, Tang F, Su W, Zhu X, Sun J, Quan R, Yang T, Han H, He J. The prevalence and survival of pulmonary hypertension due to left heart failure: A retrospective analysis of a multicenter prospective cohort study. Front Cardiovasc Med. 2022 Aug 2;9:908215. doi: 10.3389/fcvm.2022.908215. PMID: 35983183; PMCID: PMC9378855.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#动脉高压#
51
#ASC#
42
#心衰竭#
39
#患病率#
47
#生存率#
46
#Med#
28