Dig Liver Dis:血清胆固醇水平可以预测接受经颈静脉肝内门体分流术的肝硬化患者的无移植生存率
2021-12-30 MedSci原创 MedSci原创
胆固醇一种环戊烷多氢菲的衍生物。化学式为C27H46O。为白色或淡黄色结晶,是哺乳动物中主要的甾体类化合物,在基本的细胞生命活动中起到重要作用。
作为正常情况下脂质生物合成和储存的主要场所,肝脏在脂质代谢中发挥着重要作用。食物的摄入影响着血清中胆固醇和甘油三酯的水平。但禁食一段时间后,这些水平主要通过脂肪组织中的脂肪分解和肝脏中的脂蛋白颗粒合成来维持。营养不良和代谢紊乱在肝硬化中很常见,胆固醇和甘油三酯水平的下降与肝功能障碍的严重程度相关。营养状况与预后不良有关,是失代偿期肝硬化并发症增加的一个因素。此外,一些研究表明,血清胆固醇与高密度脂蛋白(HDL-C),脂蛋白(HDL-C)和低密度脂蛋白(LDL-C)的水平是肝硬化患者生存率的独立预测指标。

经颈静脉肝内门静脉分流术(TIPS)是治疗门静脉高压相关并发症的一线治疗方案。终末期肝病模型(MELD)目前已成为最广泛的用于预测接受TIPS治疗的肝硬化患者的90天生存率的工具。然而,该评分缺乏一个客观参数来衡量患者的营养状况,这可能导致低估了营养不良患者的TIPS后死亡风险。血清胆固醇可能是一个独立的营养状况和肝功能的生化参数,是预测接受TIPS治疗的肝硬化患者生存的独立指标。因此,纳入该指标可以改善目前的死亡率评分的预测能力。本研究的主要目的是评估血清胆固醇水平的预后价值。
研究人员对 2008 年至 2019 年间接受 TIPS 的肝硬化患者进行了一项探索性横断面研究。研究人员将 TIPS 前的肝移植或肝细胞癌的受试者排除本项研究。根据临床和分析数据,使用风险分析来比较所有患者的生存率。添加到MELD的血清胆固醇的诊断性能在外部验证队列中得到评估和确认。
研究结果显示:100 名患者的平均 MELD 评分为 14±5,胆固醇为 122±51 mg/dL。MELD ( p<0.05) 和胆固醇 ( p<0.05) 和低密度脂蛋白水平 (LDL-C) ( p<0.05) 都是 TIPS 后无移植存活率的独立预测因子,其中血清胆固醇的临界值为106 mg/dL。联合 MELD 胆固醇风险评分分别提高了每个参数的诊断准确性,这在外部队列中得到了证实。
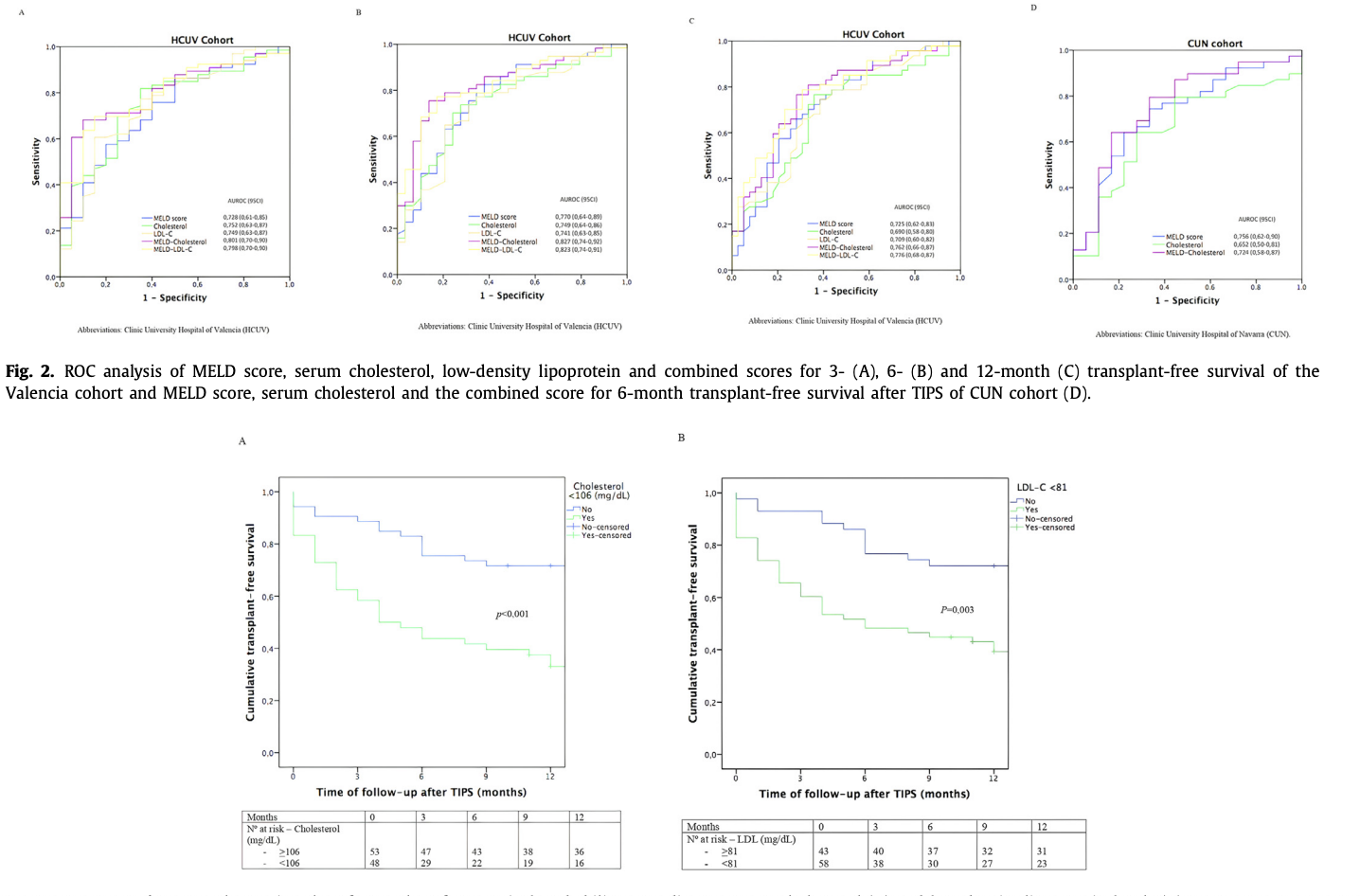
本项研究通过前瞻性的队列研究证实血清胆固醇和 LDL-C 是接受 TIPS 的肝硬化患者无移植生存的独立预测因子。MELD-胆固醇评分略微提高了预后准确性。
原始出处:
Maria PilarBallester. Et al. Serum cholesterol predicts transplant-free survival in cirrhotic patients undergoing transjugular intrahepatic portosystemic shunt. Digestive and Liver Disease.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#门体分流#
48
#Dis#
33
#静脉#
38
#经颈静脉肝内门体分流术#
61
#生存率#
50