NEJM:T细胞淋巴瘤
2015-06-22 MedSci MedSci原创
一名57的男子来院就诊,诉称其鼻子上出现结痂病变已有2个月余(如图A所示)。目前,鼻腔内偶尔会有血性的分泌物流出,但没有疼痛感及伴随其他的症状。计算机断层扫描检查未见有淋巴结肿大或转移的现象。无骨髓转移的迹象。经取多个部位组织活检,最终确诊该男子患有皮肤T细胞淋巴瘤。该男子经过一个疗程的放疗治疗后,症状明显消失(如图B所示)。三个月后,该男子出现了共济失调的症状。再次通过计算机断层扫描检查发现,其
一名57的男子来院就诊,诉称其鼻子上出现结痂病变已有2个月余(如图A所示)。
目前,鼻腔内偶尔会有血性的分泌物流出,但没有疼痛感及伴随其他的症状。计算机断层扫描检查未见有淋巴结肿大或转移的现象。无骨髓转移的迹象。经取多个部位组织活检,最终确诊该男子患有皮肤T细胞淋巴瘤。

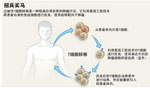
皮肤T细胞淋巴瘤(cutaneous T-cell lymphoma, CTCL)属于结外非何杰金淋巴瘤(Non-Hodgkin’s lymphoma, NHL)中的一种,是原发于皮肤的由T淋巴细胞克隆性增生造成的疾病,由一组临床表现、组织学特征、及病程预后各不相同的疾病组成。皮肤T细胞淋巴瘤占所有原发性皮肤淋巴瘤的75%-80%。近十年来,随着人们对淋巴瘤认识的深入,一些新的类型被发现,同时淋巴瘤的分型在不断的更新和进步。与其他部位的淋巴瘤相比,皮肤淋巴瘤的皮损易于发现并能及时进行活检,在疾病的诊断、分类及治疗方面发挥着重要作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#细胞淋巴瘤#
33
看看
134
图片真是醉人
105
好恶心
112
图片恶心呵呵
105
知识很不错进步
82
#T细胞淋巴瘤#
43