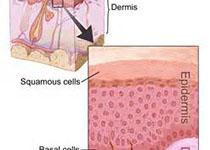
Ann Intern Med:皮肤原发性基底细胞癌的治疗比较
2018-09-19 xing.T MedSci原创
由此可见,手术治疗和外部放射治疗对于低风险的BCC复发率较低,但与其它治疗相比,其相对有效性存在很大的不确定性。在高风险BCC亚型和重要结局(包括成本)方面仍然存在差距。
大多数基底细胞癌(BCC)干预措施尚未在随机试验中进行比较。近日,内科学权威杂志Annals of Internal Medicine上发表了一篇研究文章,研究人员旨在比较原发性BCC治疗手段有效性和安全性。
该研究的数据来自MEDLINE、Cochrane对照试验中心登记处、Cochrane系统评价数据库以及Embase,检索时间从数据库成立之时到2018年5月。研究人员选择了目前用于原发性BCC治疗的比较研究。一名研究者提取了复发、组织学清除、临床清除、美容结局、生活质量和死亡率的数据,第二位评价员验证了提取数据。另一些研究者评估了每项研究的偏倚风险。
40项随机试验和5项非随机研究比较了9个类别的18项干预措施。研究人员使用频率论网络荟萃分析估计了相对干预效应和平均结局频率。手术切除(3.8%[95%CI为1.5%-9.5%])、Mohs手术(3.8%[95%CI为0.7%至18.2%])、刮除术和透热疗法(6.9%[(95%CI为0.9%-36.6%])和外部辐射(3.5%[95%CI为0.7%-16.8%])估计的复发率相似。冷冻治疗(22.3%[95%CI为10.2%-42.0%])、刮宫和冷冻治疗(19.9%[95%CI为4.6%-56.1%])、5-氟尿嘧啶(18.8%[95%CI为10.1%-32.5%])、咪喹莫特(14.1%[95%CI为5.4%-32.4%])和使用甲基氨基乙酰丙酸(18.8%[95%CI为10.1%-32.5%])或氨基乙酰丙酸(16.6%[95%CI为7.5%-32.8%])的光动力疗法复发率较高。使用甲基氨基乙酰丙酸(93.8%[95%CI为79.2%-98.3%])或氨基乙酰丙酸(95.8%[95%CI为84.2%-99.0%])光动力疗法且报告良好或更好美容效果的患者比例高于手术切除(77.8%[95%CI为44.8%-93.8%])或冷冻疗法(51.1%[95%CI为15.8%-85.4%])患者。有关生命质量和死亡率的数据太少,无法用于定量合成。
由此可见,手术治疗和外部放射治疗对于低风险的BCC复发率较低,但与其它治疗相比,其相对有效性存在很大的不确定性。在高风险BCC亚型和重要结局(包括成本)方面仍然存在差距。
原始出处:
Aaron M. Drucker,et al.Treatments of Primary Basal Cell Carcinoma of the Skin: A Systematic Review and Network Meta-analysis FREE. Ann Intern Med 2018.http://annals.org/aim/fullarticle/2702474/treatments-primary-basal-cell-carcinoma-skin-systematic-review-network-meta
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#基底细胞#
31
#细胞癌#
31
#原发性#
34
#Med#
27
#治疗比较#
33
学习了
63