EMBO Rep:铂激活Toll样受体4且有助于顺铂诱导的耳毒性
2021-04-09 AlexYang MedSci原创
Toll样受体4(TLR4)能够识别细菌脂多糖(LPS),也可被一些9/10族过渡金属激活,被认为能够介导免疫超敏反应。
Toll样受体4(TLR4)能够识别细菌脂多糖(LPS),也可被一些9/10族过渡金属激活,被认为能够介导免疫超敏反应。

最近,研究人员调查了TLR4是否可以被第10组金属铂和基于铂的化疗药物顺铂激活。

顺铂在儿童癌症治疗中是非常有价值的,但由于会引起永久性听力损失(顺铂诱导的耳毒性,CIO),其使用受到限制。研究人员在研究中阐述了铂和顺铂能够激活TLR4的下游通路,且与已知的TLR4激动剂LPS和镍具有相似的程度。研究人员进一步证明,TLR4是体外毛细胞中顺铂诱导的炎症、氧化和细胞死亡反应所必需的,也是体内毛细胞损伤所必需的。最后,研究人员鉴定了一种TLR4小分子抑制剂,其能够在体外抑制顺铂的毒性。
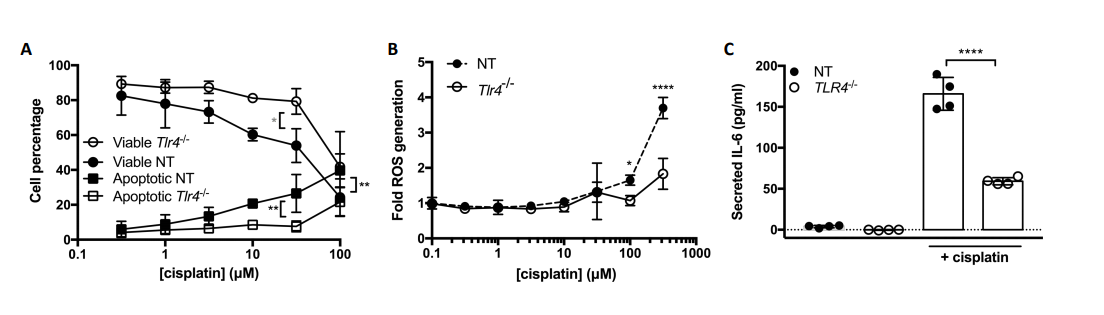
Tlr4缺失减弱了顺铂诱导的耳毒性反应
最后,他们的研究结果表明,TLR4是减轻CIO的一个很有应用前景的治疗靶点。
原始出处:
Ghazal Babolmorad , Asna Latif , Ivan K Domingo et al. Toll-like receptor 4 is activated by platinum and contributes to cisplatin-induced ototoxicity. EMBO Rep. Mar 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#铂#
41
#顺铂诱导#
42
#耳毒性#
35
好,已阅!
78
好文章!
0