Clin Trans Gastroenterology:口服质子泵抑制剂在消化性溃疡出血中可能与静脉注射一样有效
2021-04-16 MedSci原创 MedSci原创
上消化道出血的常由消化性溃疡导致(PUB),而且死亡率也比较高,大约在3%-14%左右。
上消化道出血的常由消化性溃疡导致(PUB),而且死亡率也比较高,大约在3%-14%左右。目前PUB的治疗基于两种方法:紧急内窥镜检查,必要时进行内窥镜止血和之后的保守治疗。而2015年的《欧洲胃肠道内窥镜检查指南》谨慎地建议,如果患者的病情允许,在能够耐受口服药物的患者中,高剂量口服PPI可能是一种替代选择。因此,本项研究旨在比较口服和静脉注射PPI在PUB中的疗效。
研究人员在4个数据库中对所有的相关的随机对照试验研究进行了检索,比较了口服PPI治疗与静脉(IV) PPI治疗PUB的结果。主要观察结局为30天复发性出血和30天死亡率,计算二者的95%置信区间(CI)的几率(OR)。
总共有14项随机对照试验符合纳入标准,总共收集了1,951例消化性溃疡患者,其中977例和974例分别在对照组和干预组中。口服PPI和静脉注射PPI的30天再出血率之间无统计学差异(OR = 0.96,95%CI:0.65-1.44)。30天死亡率(OR = 0.70,CI:0.35-1.40);住院时间(WMD = −0.25,95%CI:−0.93-–0.42);输血要求(WMD = -0.09,95%CI:-0.07-0.24); 需要手术(OR = 0.91,95%CI:0.40–2.07)以及进一步的内镜治疗(OR = 1.04,CI:0.56-1.93)的需求均无明显差异。
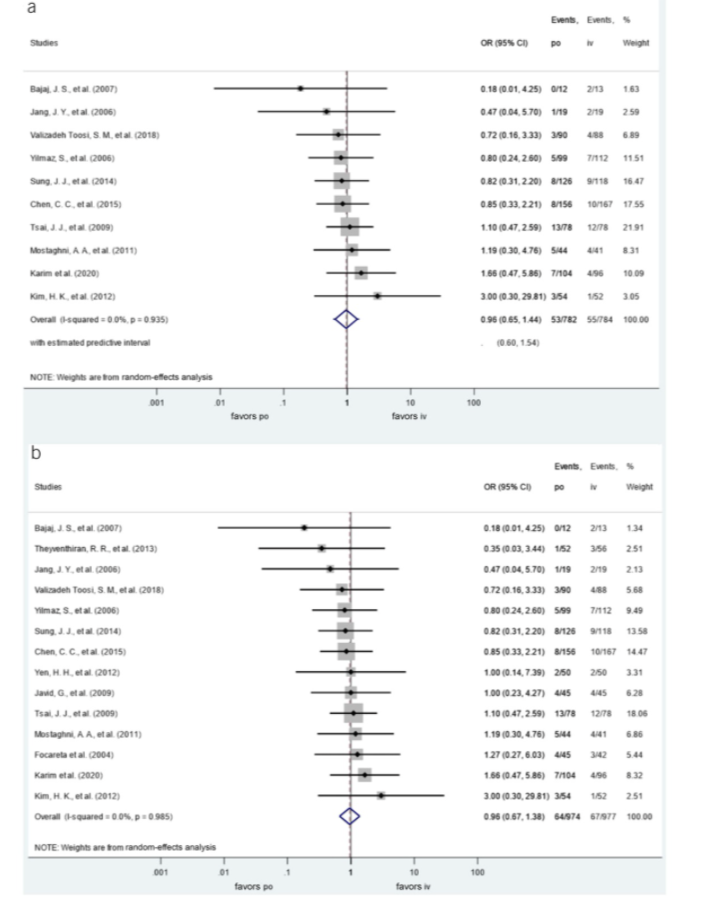
图:荟萃分析各项研究的异质性
通过本项研究证实对于消化道出血的患者经内镜治疗后口服PPI并不逊于静脉 PPI治疗,但有必要做进一步的研究。
原始出处 :
Csiki, Endre. Et al. Oral Proton Pump Inhibitors May Be as Effective as Intravenous in Peptic Ulcer Bleeding: A Systematic Review and Meta-analysis. Clinical and Translational Gastroenterology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抑制剂#
35
#静脉#
37
#质子泵#
30
#TRA#
40
#AST#
34
#GAS#
36
#Gastroenterol#
37
不错,学习了
73
#消化性溃疡#
48
#静脉注射#
29