JAMA Netw Open:列腺癌年龄分层筛查时优先选用病理活检还是磁共振成像?
2021-03-12 MedSci原创 MedSci原创
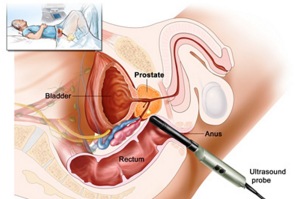
在病理活检前使用核磁共振成像(MRI)作为一种分诊检查,已被证明具有许多益处,包括使大约三分之一的男性避免了不必要的活检。
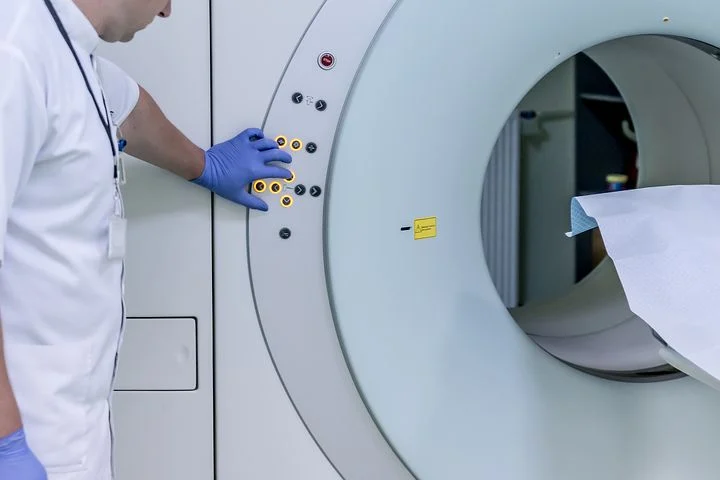
pixabay.com
对于临床怀疑患有前列腺癌的男性,在病理活检前使用核磁共振成像(MRI)作为一种分诊检查,已被证明具有许多益处,包括使大约三分之一的男性避免了不必要的活检。
尽管进行前列腺特异性抗原(PSA)筛查可以降低20%的前列腺癌特异性死亡率,但对大多数男性来说,过度诊断和过度治疗的危害被认为大于这一好处。因此,目前任何司法管辖区都不建议进行正式的、基于人群的筛查。
先前的一项模型研究表明,基于年龄和多基因图谱的风险分层筛查方案可能更具成本效益,并保留了与PSA基于年龄筛查相关的死亡率优势,同时减少癌症过度诊断的数量。然而,与优先进行活检风险分层筛查相比,活检前磁共振成像(MRI)是否与改善的利-弊和成本-效果相关?如果磁共振成像(MRI)能减轻前列腺癌的过度诊断,同时提高临床重要病例的检出率,那么可以考虑将MRI纳入前列腺癌筛查计划。
基于此,有研究者利用年龄和风险分层筛查策略,评估了活检前MRI与首次活检筛查前列腺癌相关的利弊概况和成本效益。该研究结果近日发表在JAMA Network Open期刊上。

该决策分析模型采用生命表方法,于2019年12月至2020年7月期间进行。研究人员对英国448万55岁至69岁的男性进行了分析,并随访至90岁。假设队列中无筛查、基于年龄的筛查和风险分层筛查。以年龄为基础的筛查包括每4年在55岁至69岁患者中筛查一次前列腺特异性抗原。风险分层筛选使用年龄和多基因风险谱。
分析了受益损害概况(前列腺癌死亡、质量调整生命年、过度诊断和活检)和成本效益(从卫生保健系统的角度来看,净货币收益)。基于年龄和风险分层的筛查均采用活检优先和MRI优先诊断途径进行评估。并以每年3.5%的折现率计算。
这个假设的队列最后纳入448万名英格兰男性,年龄从55岁到69岁(中位数为62岁)。与活检优先年龄筛查相比,MRI优先年龄筛查与前列腺癌死亡减少0.9%相关,过度诊断减少14.9%,活检减少33.8%。在10年绝对风险阈值为2%和10%时,MRI优先风险分层筛查与过度诊断减少10.4%和72.6%相关,MRI和活检分别减少21.7%和53.5%。在每个质量调整生命年获得20000(26000美元)和30000(39000美元)的支付意愿阈值下,最具成本效益的策略是MRI优先风险分层筛查,10年绝对风险阈值分别为8.5%和7.5%。

通过诊断途径过度诊断的癌症和前列腺癌死亡
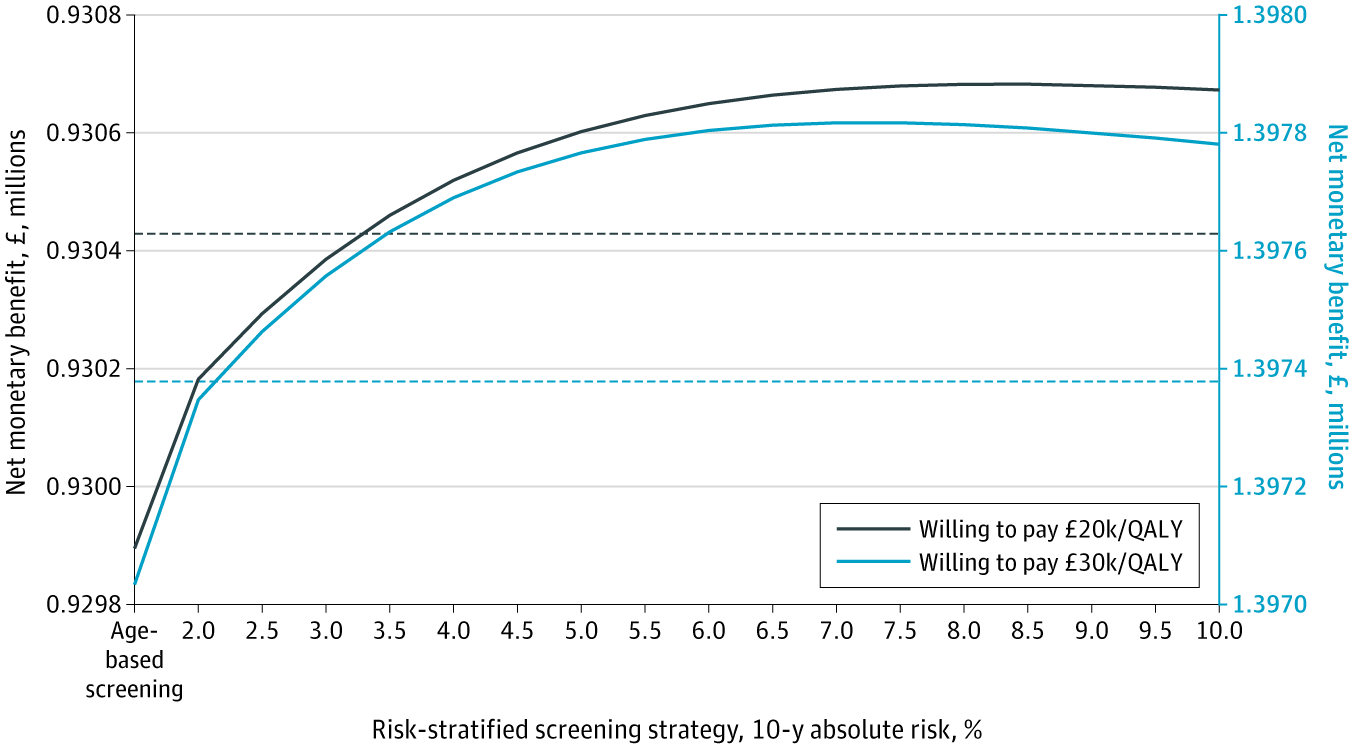
用磁共振成像优先诊断途径评估与年龄、风险分层和无筛查策略相关的净金钱效益
总之,在这个假设队列的决策分析模型中,与活检优先筛查相比,MRI优先诊断途径与前列腺癌筛查的利-弊特征和成本效益的改善相关。当使用基于年龄和多基因风险状况的风险分层筛查时,这些改善更大,当然,这些结果需要进一步的前瞻性研究来评估。
参考文献:Callender T, Emberton M, Morris S, Pharoah PDP, Pashayan N. Benefit, Harm, and Cost-effectiveness Associated With Magnetic Resonance Imaging Before Biopsy in Age-based and Risk-stratified Screening for Prostate Cancer. JAMA Netw Open. 2021;4(3):e2037657. doi:10.1001/jamanetworkopen.2020.37657
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
41
#NET#
27
#活检#
28
#磁共振#
26
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
49