Cell:宋尔卫团队揭示成纤维细胞亚群调控肿瘤干细胞新机制
2018-01-26 BioArt BioArt
“岩”是中医对癌症的描述。我们的祖先很早就认识到“质硬如石”是恶性肿瘤的重要临床特征。但肿瘤细胞本身并不硬,“质硬”是由于肿瘤微环境中成纤维细胞激活分泌胶原所致。因此,成纤维细胞激活是恶性肿瘤的共同特性。早期研究发现成纤维细胞促进肿瘤发生发展,提示其可能是良好的治疗靶点。但近期的临床试验发现,针对成纤维细胞的治疗反而加速癌症病人的病情发展。因此,既往研究提示肿瘤相关成纤维细胞具有高度的异质性。但与
“岩”是中医对癌症的描述。我们的祖先很早就认识到“质硬如石”是恶性肿瘤的重要临床特征。但肿瘤细胞本身并不硬,“质硬”是由于肿瘤微环境中成纤维细胞激活分泌胶原所致。因此,成纤维细胞激活是恶性肿瘤的共同特性。早期研究发现成纤维细胞促进肿瘤发生发展,提示其可能是良好的治疗靶点。但近期的临床试验发现,针对成纤维细胞的治疗反而加速癌症病人的病情发展。因此,既往研究提示肿瘤相关成纤维细胞具有高度的异质性。但与其他炎症细胞不同,成纤维细胞缺乏有效分群的表面标记物。如何分选和特异靶向不同成纤维细胞亚群成为目前肿瘤微环境研究领域的前沿热点问题。
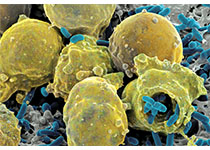
1月26日,中山大学孙逸仙纪念医院宋尔卫、苏士成团队在Cell杂志在线发表了题为“CD10+GPR77+ Cancer-Associated Fibroblasts Promote Cancer Formation and Chemoresistance by Sustaining Cancer Stemness”的研究论文。该研究率先运用细胞膜蛋白CD10和GPR77为化疗耐受相关的成纤维细胞亚群贴上“身份标签”,发现了一种新型表达CD10+与GPR77+细胞表面标记分子的癌症相关成纤维细胞,此种成纤维细胞可显着促进乳腺癌与肺癌病人对化疗的耐药性,并为肿瘤干细胞的干性维持提供了环境。
癌症相关成纤维细胞(Carcinoma-associated fibroblasts,CAFs)在肿瘤形成与癌症治疗靶点的筛选中都起到了重要作用。然而,CAFs具有异质性,并包含了众多表型与功能不一的亚群,有部分研究以CAF胞内细胞因子的表达来界定其亚群分类,但CAFs细胞相关表面分子标记的研究缺乏的阻碍了肿瘤的研究与治疗的应用。
肿瘤干细胞(Cancer stem cells,CSCs)是肿瘤的发生发展与耐药性的关键因素,其所表达的分子标记尚不明确。CSCs特异性的维持需要特殊环境的维持。虽然CAFs是CSCs干性维持环境的重要成员, 然而只有乳腺癌中分离出的CAFs可促进CSCs的聚集,其作用机理并没有解决。
既往关于成纤维细胞数目和病人预后的报道相互矛盾,提示既往的临床模型难以研究肿瘤相关成纤维细胞的异质性。该研究率先采用术前化疗作为研究肿瘤微环境异质性的临床模型。发现未经治疗的术前穿刺标本中,成纤维细胞数目与日后的术前化疗敏感性无关。但是,经过术前化疗后,耐药标本的成纤维细胞数目明显高于敏感标本。同时,耐药标本的分离成纤维细胞能诱导共培养的肿瘤细胞耐药,而敏感标本分离的成纤维细胞则不能。通过对比耐药和敏感标本成纤维细胞的表达谱,该研究利用CD10、GPR77这两个差异表达的膜蛋白,鉴定出一个CD10+GPR77+ 成纤维细胞亚群。并发现这类型的成纤维细胞数目与乳腺癌及肺癌病人的预后和化疗敏感性相关。该研究首次通过临床标本高通量筛选发现的膜蛋白鉴定成纤维细胞亚群。
CD10+GPR77+成纤维细胞的密度与乳腺癌患者术前化疗耐受及肿瘤干细胞的富集显着相关
从分子机理角度讲:CD10+GPR77+ 成纤维细胞亚群通过IL-6与IL-8维持肿瘤干细胞干性,从而导致肿瘤化疗耐药。IL-6和IL-8的分泌由持续激活的NF-kB信号调控。有趣的是,在这群细胞中NF-kB的持续激活不依赖IkB的降解。进一步研究发现,肿瘤微环境中的C5a作用于其受体GPR77,使下游RSK-1磷酸化,进而介导了非IKK依赖的p65 Ser536磷酸化。而该位点的磷酸化是p300介导的p65 lys310乙酰化的基础。p65乙酰化导致p65持续滞留在细胞核内,导致了NF-kB信号的持续激活。该研究首次阐述了补体分子对炎症转录因子转录后修饰的调控作用。
GPR77之前在成纤维细胞中的作用没有报道,那么靶向GPR77是否具有治疗价值?为了最大程度地模拟病人的肿瘤微环境,研究者采用了病人来源异质瘤(PDX)的动物模型。将富含CD10+GPR77+ 成纤维细胞的人肿瘤标本移植到小鼠脂肪垫,进而使用GPR77的阻断抗体进行治疗。实验结果显示,靶向GPR77减少肿瘤干细胞的数目和增强肿瘤化疗敏感性。因此,该研究为靶向肿瘤干细胞微环境的治疗提供了新思路。
据悉,苏士成、陈嘉宁和姚和瑞为本文共同第一作者,宋尔卫是通讯作者,中山大学是唯一作者单位。宋尔卫、苏士成团队长期致力于肿瘤微环境调控肿瘤细胞可塑性,取得了一系列系统性创新研究成果,其中包括在Cancer Cell、Cell Research、Cancer research 等国际著名期刊发表的多篇代表性论文。
原始出处:
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Cell#
27
#CEL#
26
#成纤维细胞#
23
#纤维细胞#
28
谢谢分享.学习了
44