Acta Obstet Gynecol Scand:妊娠24-31周自然分娩的头位单胎的分娩途径和结局——EPIPAGE-2队列研究
2021-07-14 MedSci原创 MedSci原创
Etude Epidémiologique sur les Petits Ages Gestationnels 2是一项法国全国性、前瞻性、基于人群的早产儿队列研究,旨在调查计划中的分娩
Etude Epidémiologique sur les Petits Ages Gestationnels 2是一项法国全国性、前瞻性、基于人群的早产儿队列研究,旨在调查计划中的分娩方式和新生儿的结果与头位自然早产之间的关系,研究结果已发表于Acta Obstet Gynecol Scand。
研究纳入了单胎头胎妊娠和自发早产或妊娠24-31周胎膜早破的妇女。主要暴露是计划中的分娩方式(即计划中的阴道分娩或开始分娩时计划中的剖腹产)。主要结果是出院时的存活率,次要结果是出院时无严重病症的存活率。使用倾向性评分来最小化估计关联的指示性偏差。
结果,研究共纳入1008名妇女:206名(20.4%)计划剖腹产,802名(79.6%)计划阴道分娩。总共有723人(90.2%)最终采用了阴道分娩。总的来说,计划剖腹产组和计划阴道分娩组的187名(92.0%)和681名(87.0%)新生儿活着出院,156名(77.6%)和590名(76.3%)活着出院,没有严重发病。在倾向性评分匹配后,计划性剖宫产与生存率(aOR 1.05,95% CI 0.48-2.28)或无严重病症的生存率(aOR 0.64,95%CI 0.36-1.16)无关。
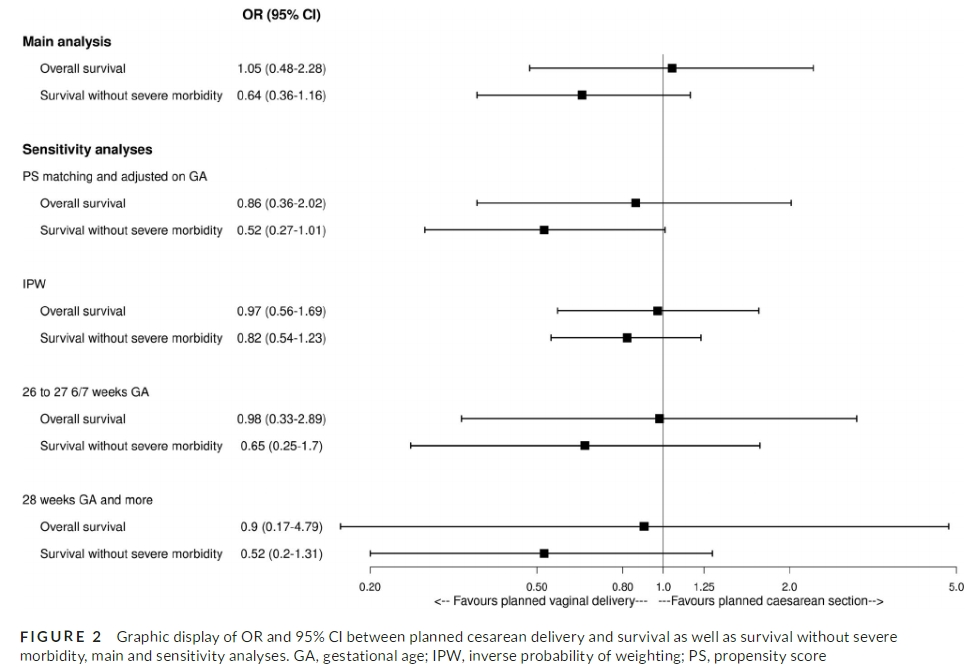
综上所述,该研究结果表明,早产或胎膜早破后在妊娠24-31周计划性剖腹产头位并不能改善新生儿的结局。
原始出处:
Adrien Gaudineau, et al., Planned delivery route and outcomes of cephalic singletons born spontaneously at 24-31 weeks' gestation: The EPIPAGE-2 cohort study. Acta Obstet Gynecol Scand. 2020 Dec;99(12):1682-1690. doi: 10.1111/aogs.13939.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#NEC#
33
#TET#
0
#CTA#
28
#分娩#
43