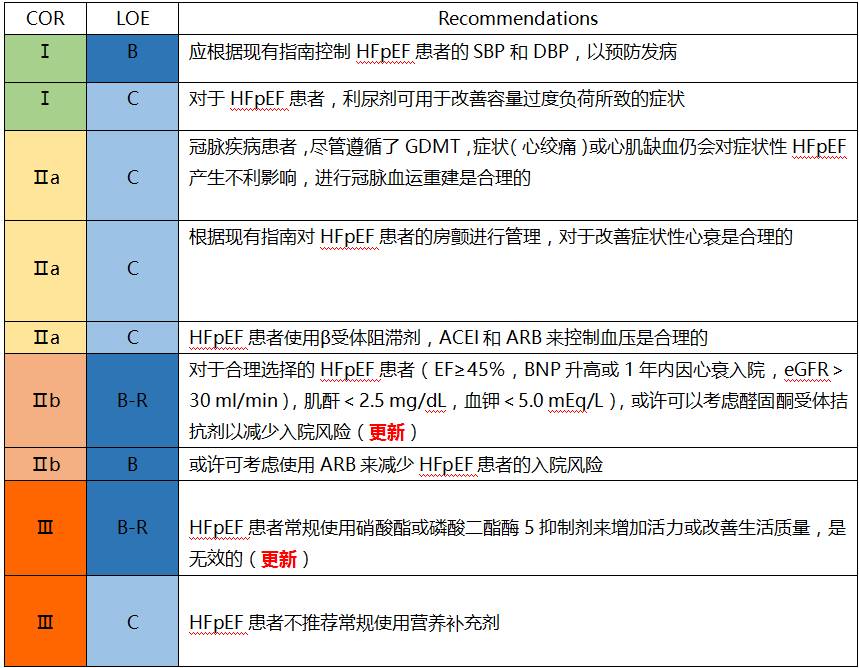
GW-ICC2017︱余静:慢性心力衰竭合并高血压患者的血压管理
2017-10-13 余静 国际循环
在本届GW-ICC 2017的心衰合并症的诊治论坛上,来自兰州大学第二医院的余静教授就慢性心衰患者合并高血压患者的血压管理问题作了精彩的专题报告。下面带领您一览该报告的精彩内容。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#慢性心力衰竭#
37
#血压管理#
42
#高血压患者#
39
#ICC#
38
#GW-ICC#
41
好好学习好好学习天天向上
60
很好很好很好
73
学习.
57
学习了
67
学习了.谢谢.
55