Nat Commun:科学家揭示动脉粥样硬化调控新机制
2019-01-28 李惠钰 中国科学报
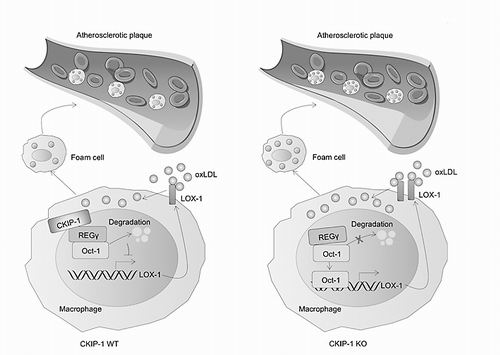
日前,记者从军事科学院军事医学研究院某研究所获悉,该所国家蛋白质科学中心(北京)张令强团队首次报道酪蛋白激酶2相互作用蛋白1(CKIP-1)在动脉粥样硬化过程中的保护性作用及分子机制。相关研究成果在1月25日出版的《自然—通讯》杂志发表。CKIP-1最初作为CK2激酶的结合蛋白而被发现,张令强团队对此分子开展了近20年深入研究,先后阐明了其在调控骨发育与骨质疏松症、心脏发育与心肌肥大、肿瘤发生发展
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#COMMUN#
20
学习了
70
#Nat#
20
#粥样硬化#
21
科学家揭示动脉粥样硬化调控新机制。
67
科学家揭示动脉粥样硬化。
55