J Clin Oncol:纳武单抗治疗晚期NSCLC的5年随访预后仍明显优于多西他赛!
2021-01-21 MedSci原创 MedSci原创
纳武单抗治疗晚期NSCLC的5年随访预后仍明显优于多西他赛!
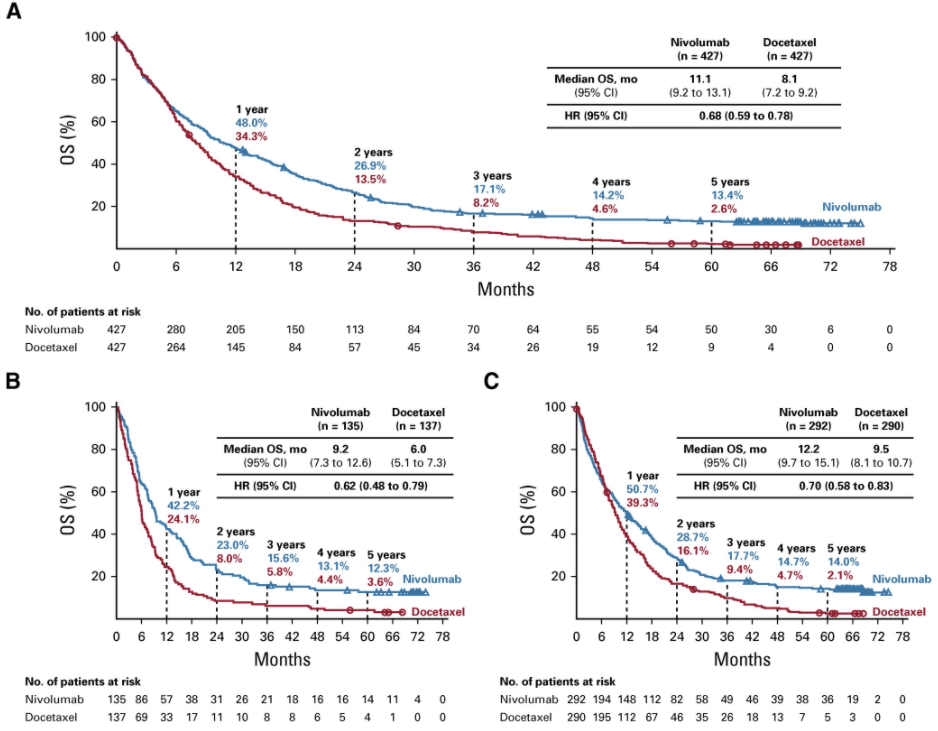
免疫疗法为晚期非小细胞肺癌(NSCLC)的治疗带来了革命性的变化。在两项III期试验(CheckMate 017和CheckMate 057)中,纳武单抗与多西他赛相比,可进一步提高既往治疗过的晚期鳞状和非鳞状NSCLC患者的总存活率(OS),而且安全性也更好。本文报告了这些试验的5年汇总疗效和安全性结果。
两项试验共854位晚期NSCLC患者,ECOG PS ≤1和一线铂为基础的化疗过程中/后发生了进展,被随机分为两组,分别给予纳武单抗(3 mg/kg,1次/2周)或多西他赛(75 mg/m,1次/3周)治疗,直至进展或出现不可接受的毒性。两项试验的主要终点都是OS;次要终点包括无进展生存期(PFS)和安全性。
所有患者的OS
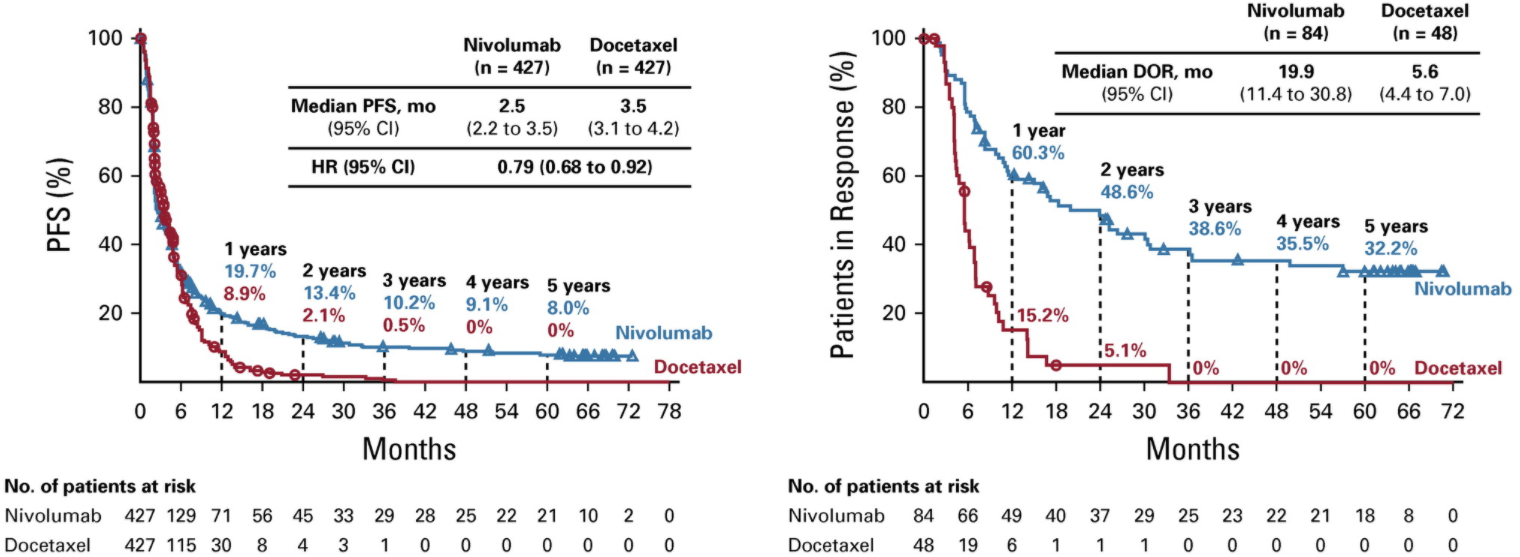
Checkmate 017和057试验分别最短随访时间了64.2和64.5个月后,接受纳武单抗治疗的患者和接受多西他赛治疗的患者分别还有50位和9位仍存活着。5年汇总OS率分别为13.4%和2.6%;5年PFS率分别为8.0%和0%。
所有患者的PFS和缓解率
接受纳武单抗治疗的2年和3年无进展的患者的存活率分别为82.0%和93.0%,5年无进展的存活率分别为59.6%和78.3%。从随访第3年到第5年期间,纳武单抗治疗的患者报告了31例与治疗相关的不良事件(TRAE),其中7人发生了新的不良事件;1例(3.2%)TRAE为3级,没有4级TRAE。
随访5年,与多西他赛相比,纳武单抗继续显示出生存益处,OS率较多西他赛治疗高了5倍,且没有新的安全事件。这是第一份关于程序性死亡蛋白1抑制剂用于既往治疗过的晚期NSCLC的III期随机临床试验的5年预后结果。
原始出处:
Borghaei Hossein,Gettinger Scott,Vokes Everett E et al. Five-Year Outcomes From the Randomized, Phase III Trials CheckMate 017 and 057: Nivolumab Versus Docetaxel in Previously Treated Non-Small-Cell Lung Cancer. J Clin Oncol, 2021, JCO2001605.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#5年随访#
47
#J Clin Oncol#点击查看更多该期刊内容
85
#Oncol#
29
#晚期NSCLC#
41
#非小细胞肺癌#
116
谢谢梅斯分享这么多精彩信息
55
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
35