Lancet oncol:70基因组合可很好的鉴别低基因组风险的乳腺癌患者!
2021-03-16 MedSci原创 MedSci原创
MINDACT试验的延长随访结果来了~
MINDACT试验显示,未接受化疗的高临床和低基因组风险的乳腺癌患者有很高的5年无远处转移生存率(94.7%,95%CI 92.5–96.2)。本次分析阐述了长期随访结果以及按年龄进行的探索性分析。
MINDACT试验是一项在欧洲9个国家112个医疗学术中心开展的多中心、随机的3期试验,招募了18-70岁的组织学确诊的原发性侵袭性乳腺癌患者(分期为T1期、T2期或T3期),至多有3个淋巴结转移,无远处转移,WHO表现状态评分0-1分。采用MammaPrint 70-基因组合评估基因组风险,采用校正版的Adjuvant!Online评估临床风险。受试患者1:1随机分组基于临床风险或基因组风险接受化疗或不化疗。主要终点是5年无远处复发生存率。
研究流程
2007年2月8日-2011年7月11日,共招募了6693位患者。截止2020年2月26日,中位随访了8.7年。未进行化疗的高临床风险、低基因组风险的患者的最新的5年无远处转移生存率为95.1%(95%CI 93.1-96.6),超出了预定的非劣效性界值92%,支持既往分析并证明MINDACT试验是一个有效的降级试验。
4个风险组的无远处转移生存率
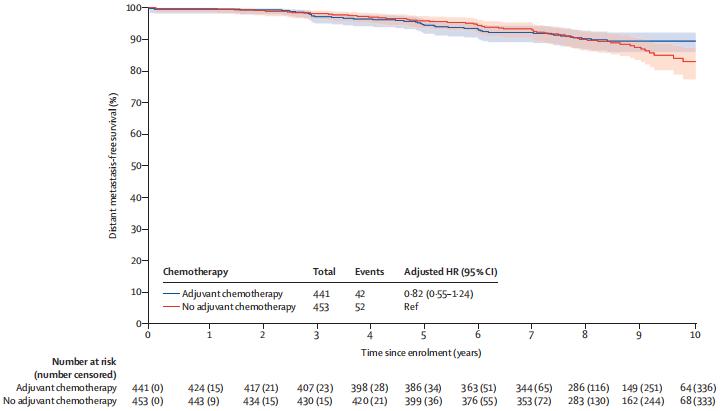
高临床风险和低基因组风险患者(意向治疗人群)随机接受化疗(n=749)或不接受化疗(n=748)。在意向治疗人群中,化疗组和无化疗组的估计8年无远处复发生存率分别为92.0%(95%CI 89.8-93.8)进而89.4%(86.8-91.5;风险比[HR] 0.66,95%CI 0.48-0.92)。
≤50岁的患者的无远处转移生存率
仅限于激素受体阳性、HER2阴性的患者亚组(化疗组676人、无化疗组 682人)的探索性分析显示,在不同年龄的患者中,化疗对8年无远处转移生存率的效应不同:在≤50岁的患者中,化疗组和无化疗组的8年无远处转移生存率分别为93.6%和88.6%(绝对差5.0%);在>50岁的患者中,化疗组和无化疗组的8年无远处转移生存率分别为90.2%和90.0%(绝对差0.2%)。
>50岁的患者的无远处转移生存率
在无淋巴结转移(n=699)的患者中,化疗组和无化疗组的8年无远处转移生存率分别为91.7%和89.2%(绝对差2.5%);在有1-3个淋巴结转移的患者(n=658)中,化疗组和无化疗组的8年无远处转移生存率分别为91.2%和89.9%(绝对差1.3%)。
长达9年的延长随访研究结果展示了70-基因组合鉴定高临床风险、低基因组风险患者的出色能力,鉴定出的这类患者仅采用内分泌治疗就可获得极好的无远处转移生存率。对于这类患者,内分泌治疗基础上予以化疗的增益仍较少,且不随淋巴结转移而增加。
原始出处:
Maritine Piccart, et al. 70-gene signature as an aid for treatment decisions in early breast cancer: updated results of the phase 3 randomised MINDACT trial with an exploratory analysis by age. The Lancet Oncology. March 12, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Oncol#
23
#Lancet#
27
#乳腺癌患者#
27
顶刊就是不一样,质量很高,内容精彩!学到很多
51
谢谢梅斯分享这么多精彩信息
53