Cell研究:对抗心脏病,从调节肠道菌群开始
2015-12-29 孙学军博客 科学网博客园
长期以来,大量存在于红肉(如牛肉、羊肉等)里的左旋肉碱曾一度与胆碱和卵磷脂一起被认为属于营养成分,但两年前美国的一项研究指出,左旋肉碱可能在肠道细菌作用下,由利变害,导致动脉硬化。不久前,有科学家根据这一发现,提出了通过干扰肠道细菌来预防心脏病的新思路。 之所以过去被认为是营养物质,乃至一度被各国认可作为食品强化剂的左旋肉碱和胆碱能诱发动脉硬化,原因是这类物质能被大肠内的细菌代谢产生三甲胺
长期以来,大量存在于红肉(如牛肉、羊肉等)里的左旋肉碱曾一度与胆碱和卵磷脂一起被认为属于营养成分,但两年前美国的一项研究指出,左旋肉碱可能在肠道细菌作用下,由利变害,导致动脉硬化。不久前,有科学家根据这一发现,提出了通过干扰肠道细菌来预防心脏病的新思路。
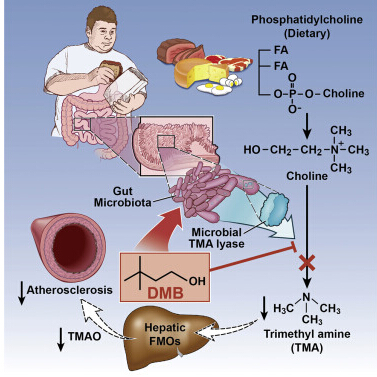
之所以过去被认为是营养物质,乃至一度被各国认可作为食品强化剂的左旋肉碱和胆碱能诱发动脉硬化,原因是这类物质能被大肠内的细菌代谢产生三甲胺,三甲胺被肠道吸收后在肝脏内被代谢成能促进动脉硬化的三甲胺N-氧化物trimethylamine-N-oxide(TMAO)。研究发现,摄取同样数量的左旋肉碱,杂食性人比素食者可产生更多的TMAO,这是因为杂食性人肠道内有特殊的细菌类型。
实验发现,给小鼠长期喂食左旋肉碱可以改变动物肠道内细菌的成份,导致血液中TMAO升高,并发生动脉硬化。如果抑制细菌的生长,则不会发生这些改变。肠道细菌是导致食用红肉诱导动脉硬化的原因。
一项对2595个人开展的流行病学调查发现,血浆中左旋肉碱的含量和心血管病发病率以及心血管严重后果之间没有直接关系。但如果血液中同时伴随TMAO升高,则左旋肉碱的含量和心血管病发病率以及心血管严重后果的发生之间存在相关关系。在发现肠道细菌的关键作用之前,人们对其内在原因并不了解。
既然肠道细菌是导致TMAO产生的一个环节,那么能不能通过药物干扰微生物代谢,减少TMAO产生,实现预防心脏病的目的呢?2015年12月17日,《细胞》(CELL)杂志就发表了一项由克利夫兰医学中心开展的研究,首次采用干扰肠道菌代谢活性的药物,提出通过调节肠道菌群来治疗心脏病的新策略。
此前,靶标这一通路的方式主要是抑制肝脏转化三甲胺的酶。但这种方式会引起肝脏损伤和三甲胺累积。最新刊登在《细胞》上的这篇论文的通讯作者Hazen及其团队找到了一个更有前景的途径,直接靶标肠道菌,从源头阻止三甲胺形成。
Hazen和论文的第一作者Zeneng Wang筛选出了能够抑制三甲胺产生的化合物3,3-二甲基丁醇DMB(3,3-dimethyl-1-butanol)。一些冷压特级初榨橄榄油、香醋和葡萄籽油天然就富含DMB。研究人员建立了小鼠动脉硬化模型,并为其提供富含胆碱的饮食。研究显示,DMB治疗能够显著降低小鼠的TMAO水平,抑制动脉斑块形成,并且没有毒副作用。
进一步研究表明,DMB确实能够通过抑制三甲胺的形成来起作用。而且DMB不杀死肠道细菌,只是降低与高水平三甲胺、TMAO和动脉硬化有关的特定细菌在肠道菌中所占的比例。“这种药物不杀死细菌但又能阻断通路,效果非常好,”Hazen说。“与抗生素相比,非致死性药物面临的选择压力更小,不那么容易引发抗性。”
DMB治疗和降胆固醇药物,如立普妥(Lipitor)不同,它靶标的是肠道菌的分子通路而不是人类细胞内的代谢酶。“这可能成为治疗心血管和代谢疾病的全新治疗策略。”
地中海式饮食以鱼类、豆类、蔬菜、水果、坚果、橄榄油为主,搭配适量红酒。这种饮食搭配近年来特别受人青睐,被认为能预防心血管疾病。克利夫兰医学中心这一研究发现,地中海式饮食通过改变肠道菌的活性来发挥健康效应。通过膳食补充一种在红酒和橄榄油中含量丰富的DMB,可防止小鼠肠道菌将不健康食品转化为堵塞动脉的代谢副产品。
对大多数人而言,通过地中海式饮食来延缓心脏病和其他健康问题,不失为一个立刻可行的主意。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
29
#CEL#
34
是一篇不错的文章
125
这篇文章有一定深度
143
这个值得关系
122
值得收藏得文章,
91
调节肠道菌群,
109
应该从饮食及生活方式出发,
117
赞,
95
不错,
93