病例报告丨罕见的胃腺癌合并倒置性增生性息肉一例
2020-06-16 董玮 姜栋栋 袁州杰 消化科空间 中华消化内镜杂志
倒置性增生性息肉在内镜下和组织病理学上都比较容易导致临床误诊,本文报道了1例胃窦腺癌合并胃窦部倒置性增生性息肉病例,结合相关文献重点,从内镜下和临床病理学特征等方面对该病变进行阐述,以期提高内镜医师和
摘要
倒置性增生性息肉在内镜下和组织病理学上都比较容易导致临床误诊,本文报道了1例胃窦腺癌合并胃窦部倒置性增生性息肉病例,结合相关文献重点,从内镜下和临床病理学特征等方面对该病变进行阐述,以期提高内镜医师和病理科医师对胃倒置性增生性息肉的认识。
患者男,68岁,因长期胃部不适行胃镜检查示:胃窦大弯侧一溃疡(图1),大小1.0 cm×1.5 cm;距溃疡4 cm处胃窦近胃体小弯侧一广基隆起,直径约1.0 cm(图2)。患者无其他恶性疾病病史,行影像学检查和评估后行胃癌根治术(胃大部切除并RY吻合术)。
病理回报:(胃窦大弯侧)溃疡型腺癌,分化中等,部分为黏液腺癌,大小1.0 cm×1.5 cm,癌组织侵达浆膜下层,侵及神经(图3),脉管内未查见明显癌栓,胃大弯淋巴结6枚、胃小弯淋巴结15枚均未查见癌转移,网膜组织和标本两端切缘均未见异型上皮;(胃窦近胃体小弯侧)倒置性增生性息肉,大小1.0 cm×1.0 cm,位于黏膜下层,外层为纤细黏膜肌包绕,呈边界清楚的倒置性内翻性生长模式(图4A),表面黏膜组织未见明显异常、病变内未见显著细胞学异型性(图4B)。
免疫组织化学检测(EnVision两步法):胃小凹上皮和颈部腺体分别呈MUC-5AC和MUC-6细胞质阳性(图5A、图5B);灶性区域少量小凹腺体(比例约8%)呈CD10腺体腔缘阳性(图5C)、CDX-2细胞核阳性(图5D)、MUC-2细胞质阳性(图5E)。Ki-67增殖指数:颈部腺上皮阳性(图5F),分别为肠型腺体表达约10%阳性、胃型腺体表达5%以下。

图1 胃窦大弯侧病灶的内镜图像,胃窦大弯侧偏前壁可见大小1.0 cm×1.5 cm的溃疡,表面覆厚白苔及血痂,周边黏膜隆起、充血水肿
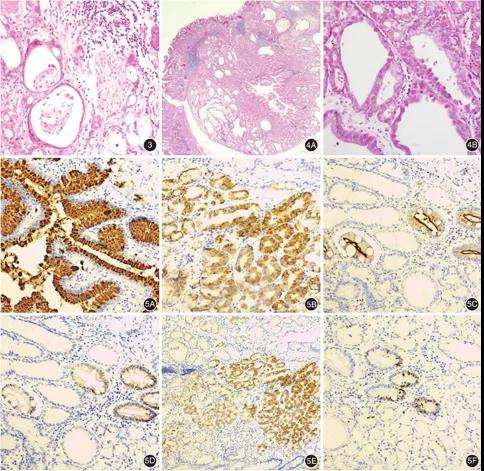
图2 胃窦近胃体小弯侧病灶内镜图,直径约1.0 cm的广基隆起,表面充血,黏膜光滑
图3 胃大部切除术后胃窦大弯侧病理,该处异型腺体呈浸润性生长,可见神经侵犯 HE ×200
图4 胃大部切除术后胃窦近胃体小弯侧病理 4A:病变呈倒置性生长,表面被覆正常胃体黏膜 HE ×40; 4B:部分腺体呈微囊性扩张,上皮细胞未见明确异型性 HE ×200
图5 胃大部切除术后胃窦近胃体小弯侧免疫组织化学检测(EnVision两步法) 5A:部分腺体呈胃小凹上皮型黏液MUC-5AC免疫组化染色阳性 ×200;5B:部分腺体呈小凹颈部型黏液MUC-6免疫组化染色阳性 ×200;5C:个别腺体呈小肠刷状缘标记CD10免疫组化染色阳性 ×200;5D:呈CD10免疫组化染色阳性的个别腺体同时呈肠上皮标记物CDX-2免疫组化染色阳性 ×200;5E:个别腺体示肠上皮黏液标志物MUC-2免疫组化染色弱阳性 ×100;5F:免疫组化染色Ki-67显示小凹颈部腺上皮阳性 ×200
讨论
胃增生性息肉是一种常见的良性上皮增生性病变,绝大多数表现为向胃腔内生长的肿块,上皮细胞无明显异型性。罕见情况下,增生性息肉呈内翻或倒置性向黏膜下层膨胀性生长,少部分病例合并胃癌发生。胃息肉按其形态可分为"突出型"或"倒置型"。绝大多数胃息肉为突出型,倒置性增生性息肉非常罕见。胃倒置性增生性息肉患者,大多数通常无明显症状。内镜下,胃倒置性增生性息肉很可能被误诊为一些向黏膜下生长的上皮性病变或起源自黏膜下层的占位性病变,如胃肠道间质瘤、神经内分泌肿瘤、平滑肌瘤、神经鞘瘤、异位的胰腺组织等。
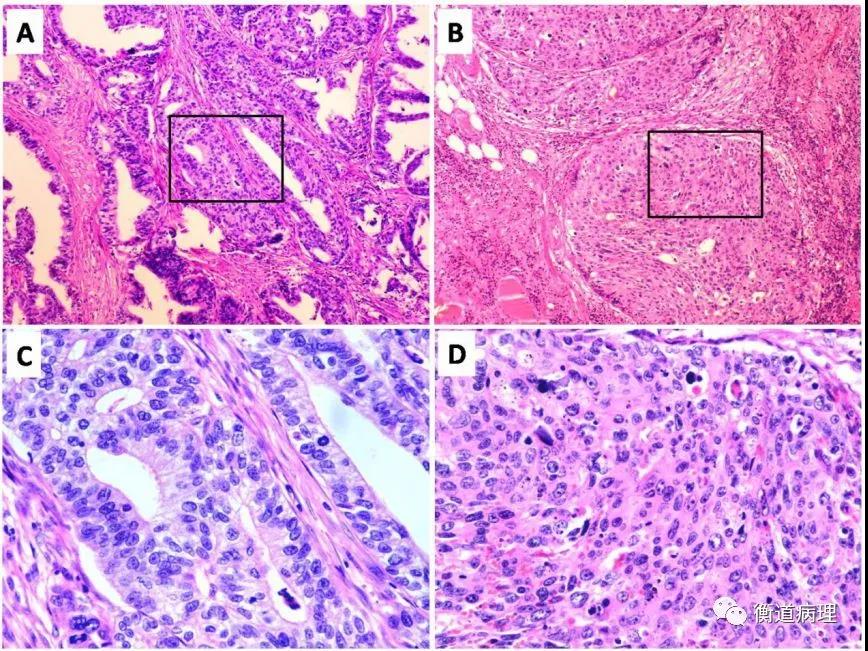
胃倒置性增生性息肉组织学特征是呈增生性息肉特征的黏膜腺体在黏膜下层明显增生,病变边界清楚,上皮细胞无明显异型性。目前共检索到12篇已公开发表的胃良性倒置性增生性息肉报道,结合本例我们对这些病例(共18例)进行了汇总分析,发现患者平均年龄为59.5岁(34~85岁),男女比例为1.25∶1,8例位于胃底、5例位于胃体、4例位于胃窦、1例息肉位于贲门,息肉大小为0.5~1.0 cm,病变均为由小凹型上皮细胞(13例)和各种胃腺体(包括幽门型2例、胃底腺3例)混合构成,在一些病例中病变内可见平滑肌束增生、肠上皮化生和肠嗜铬细胞样细胞增生。在本例中,胃倒置性增生性息肉由小凹型上皮细胞(约占36%)、胃底腺(约占56%)和肠上皮化生细胞混合构成(约92%为胃型上皮黏液表型特征,灶性8%为小肠型黏液表型),并且在不同的位置处合并胃溃疡型腺癌。共有8例合并发生了胃腺癌,其中1例同时发现了印戒细胞癌。
组织学上,胃倒置性增生性息肉应与浸润至黏膜下层的高分化腺癌相鉴别。胃倒置性增生性息肉一般边界清楚,腺体排列规则,呈简单的管状结构,细胞无异型性;而浸润至黏膜下层的高分化腺癌一般边界不清,结构复杂,呈浸润性生长,浸润到黏膜下层的异型腺体结构紊乱,周围伴有促纤维结缔组织增生,细胞核质比例增大,异型显著。另外,胃倒置性增生性息肉也要与囊性深在性胃炎相鉴别。前者一般具有明显的增生性特征,边界清楚;后者是由于黏膜腺体向下迁徙所致,腺体呈管状或微囊向下扩张。
尽管胃倒置性增生性息肉的发病机制尚不清楚,但最近的研究表明炎症和随后的愈合可能将黏膜成分挤压至黏膜下层。偶有胃倒置性增生性息肉表面被覆黏膜周围出现早期腺癌的报道。总之,胃倒置性增生性息肉是一种罕见的息肉,腺体下陷至黏膜下层,形成倒置性球形外观,息肉周围可有纤细的黏膜肌包绕,息肉腺体主要有泌酸腺、幽门腺和固有腺体特征,本身恶变罕见,但可以合并不同部位的腺癌发生。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#增生性#
48
#胃腺癌#
42
#病例报告#
51
#罕见#
45