JAMA Netw Open: 氯噻酮与氢氯噻嗪在肾功能不同的老年人中的临床结局和安全性比较
2021-09-18 MedSci原创 MedSci原创
高血压是世界范围内发病率和死亡率最大的单一因素。噻嗪类利尿剂通常用于治疗高血压,而高血压在老年人和慢性肾病患者中非常普遍。最近发表的一篇文章比较了不同肾功能水平的老年人使用氯噻酮或氢氯噻嗪的安全性和临
高血压是世界范围内发病率和死亡率最大的单一因素。噻嗪类利尿剂通常用于治疗高血压,而高血压在老年人和慢性肾病患者中非常普遍。氢氯噻嗪是北美处方最多的噻嗪利尿剂,尽管它比氯噻酮的作用更短,药效(每毫克)更低。虽然以前的研究表明氯噻酮在控制血压和减少心血管事件方面具有优势,但最近的研究表明氯噻酮在降低心血管风险方面虽具有同等作用,但其不良肾脏结局和低血钾的风险较高
最近发表的一篇文章比较了不同肾功能水平的老年人使用氯噻酮或氢氯噻嗪的安全性和临床结果。
实验方法
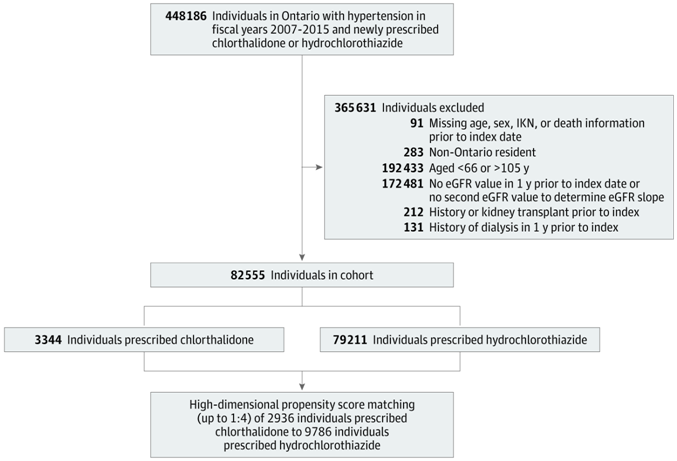
这项基于人群的回顾性队列研究于2007年至2015年在加拿大安大略省进行。参与者包括66岁或以上的成年人,在此期间服用氯噻酮或氢氯噻嗪。分析了2019年12月至2020年9月的数据。
新氯噻酮使用者与新氢氯噻嗪使用者的高维倾向评分匹配为1:4。考虑到竞争风险的时间-事件模型研究了氯噻酮 vs.氢氯噻嗪使用与总体感兴趣的结果和估计肾小球滤过率(eGFR)类别(≥60、45-59和<45 mL/min/1.73 m2)之间的关系。
感兴趣的结果是不良肾脏事件(如eGFR下降≥30%、透析或肾移植)、心血管事件(包括心肌梗死、冠状动脉重建、心力衰竭或房颤)、全因死亡率和电解质异常(如钠或钾水平超出参考值范围)。
Figure 1:研究方案
实验结果
1. 肾脏不良事件
与氢氯噻嗪相比,氯噻酮的使用与eGFR下降30%或更高的风险相关(Figure 2A)。对于透析或肾移植患者,氯噻嗪与氢氯噻嗪的使用风险没有显著差异(Figure 2B)。
Figure 2:肾脏不良事件

2. 心血管事件
与氢氯噻嗪相比,氯噻酮的使用与心血管事件的高风险相关(Figure 3A)。eGFR分类对相关性无影响。
Figure 3:心血管事件(CV)和全因死亡率

3. 全因死亡率
氯噻嗪组和氢氯噻嗪组的全因死亡率没有显著差异(Figure 3B)。然而,在eGFR为60 mL/min/1.73 m2或更高的参与者中,氯噻酮与氢氯噻嗪相比具有更高的全因死亡风险。相比之下,在eGFR为60 mL/min/1.73 m2以下的参与者中,全因死亡风险没有显著差异。eGFR类别和氯噻酮或氢氯噻嗪使用与全因死亡率之间的关系相关。
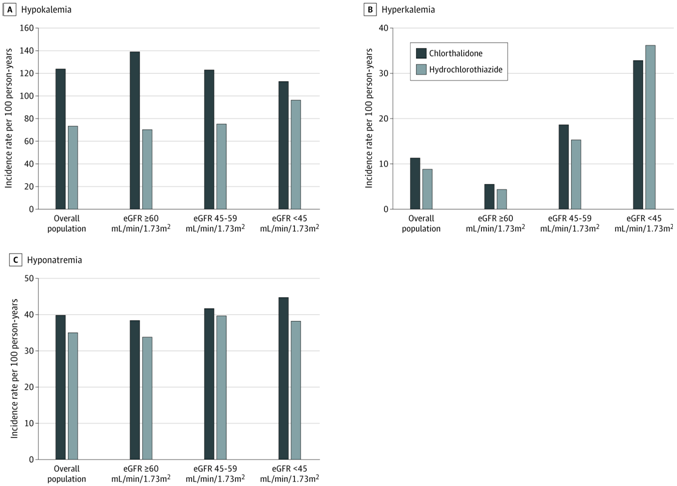
4. 电解质紊乱
与氢氯噻嗪相比,氯噻酮的使用与低钾血症的高风险相关(Figure 4A)。在基线肾功能较高的患者中,氯噻酮低钾血症风险的增加更为显著。氯噻嗪组和氢氯噻嗪组在高血钾、低血钠风险方面没有显著差异(Figure 4B 和Figure 4C)
Figure 4:电解质紊乱
结论
在这项以人群为基础的老年人队列研究中,我们发现,与氢氯噻嗪的使用相比,氯噻酮的使用与eGFR下降、心血管事件和低血钾的风险更高相关。在肾功能降低的参与者中,氯噻酮引起低钾血症的额外风险降低。与之前比较噻嗪类利尿剂安全性和临床结果的观察性研究相结合,这些结果表明,与氢氯噻嗪相比,没有明确的理由优先选择氯噻嗪。
原文链接:https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2784119
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#噻嗪#
34
#临床结局#
40
#NET#
33
#肾功能#
31
#PE#
37
#氯噻酮#
30
#氢氯噻嗪#
28