JASN:RI-CYCLO随机试验| 利妥昔单抗 vs 环磷酰胺治疗膜性肾病
2021-03-04 MedSci原创 MedSci原创
糖皮质激素-环磷酰胺方案是膜性肾病的一线治疗方案。利妥昔单抗治疗是否较该方案具有更有利的安全性?
糖皮质激素-环磷酰胺方案是膜性肾病的一线治疗方案。与该方案相比,利妥昔单抗治疗可能具有更有利的安全性,但缺乏正面的对比。
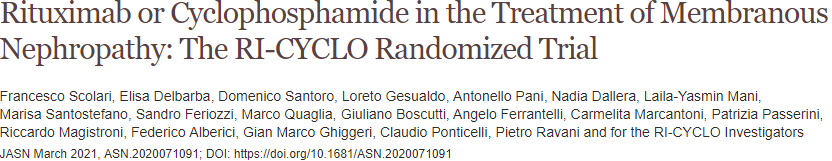
本研究将74例蛋白尿>3.5g/d的膜性肾病成人患者随机分至两组(各37人),接受利妥昔单抗(1g,第1天和第15天)或皮质类固醇+环磷酰胺交替治疗6个月。
研究方案
主要结果是12个月后蛋白尿完全缓解。次要指标包括在24个月时完全或部分缓解以及不良事件的发生。
12个月时,利妥昔单抗组和周期方案组分别有23名(62%)和27名(73%)患者获得完全或部分缓解(优势比[OR] 0.61;95%CI 0.23~1.63),其中分别有6名(16%)和12名(32%)患者获得完全缓解(OR 0.4;95%CI 0.13~1.23)。
主要预后
24个月时,利妥昔单抗组的缓解率(完全缓解+部分缓解)和完全缓解的概率分别为0.83(95%CI,0.65~0.95)和0.42(95%CI,0.26~0.62),周期方案组的分别为0.82(95%CI,0.68~0.93)和0.43(95%CI,0.28~0.61)。
利妥昔单抗组有19%的患者发生了严重不良事件,周期方案组有14%的患者发生了严重不良事件。
综上,该试验未发现,利妥昔单抗与皮质类固醇-环磷酰胺周期方案相比在膜性肾病治疗中有更多益处或更少危害的表现。
原始出处:
Scolari Francesco,Delbarba Elisa,Santoro Domenico et al. Rituximab or Cyclophosphamide in the Treatment of Membranous Nephropathy: The RI-CYCLO Randomized Trial. J Am Soc Nephrol, 2021, 10.1681/ASN.2020071091
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#利妥昔#
0
#ASN#
48
#学习#
73
学习了
63
循证
63
#环磷酰胺#
38
#随机试验#
38
高质量研究,读起来真爽,谢谢梅斯
49
学习了
83
好文章!
78