ASCO 2015:PD-1单抗治疗进展期肾癌带来生存获益
2015-06-05 佚名 中国医学论坛报今日肿瘤微信公众号
图 北京大学肿瘤医院肾癌黑色素瘤内科 崔传亮 作为目前进展期肾癌的标准治疗,靶向治疗带来的临床获益已经达到一个相对平台期。近年来,随着免疫检查点阻断药物临床数据的不断公布,免疫治疗已成为进展期肾癌患者生存进一步改善的希望。 2014年KEYNOTE-012研究已公布了nivolumab(PD-1的IgG4单克隆抗体)在进展期肾癌中的疗效。研究随机入组了168例既往VEG

图 北京大学肿瘤医院肾癌黑色素瘤内科 崔传亮
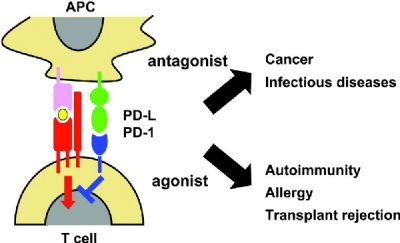
作为目前进展期肾癌的标准治疗,靶向治疗带来的临床获益已经达到一个相对平台期。近年来,随着免疫检查点阻断药物临床数据的不断公布,免疫治疗已成为进展期肾癌患者生存进一步改善的希望。
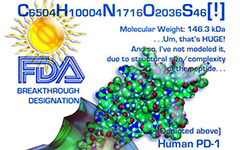
2014年KEYNOTE-012研究已公布了nivolumab(PD-1的IgG4单克隆抗体)在进展期肾癌中的疗效。研究随机入组了168例既往VEGFR-TKI耐药的进展期肾癌患者,随机进入nivolumab 0.3 mg/kg、2 mg/kg、10 mg/kg组,研究中64%的患者测定了PD-L1表达,27% 的患者阳性(膜表达≥5%)。3组患者的中位PFS为2.7、4.0、4.2个月,客观有效率20%~22%,证实了其在进展期肾癌治疗中的疗效及安全性。2015年ASCO更新了研究总生存的数据,随访至2015年1月,3组的1年生存率分别为63%、72%、70%,2年生存率分别为42%、53%、52%,3年生存率33%、40%、32%。亚组分析表明PD-L1(+)患者中位总生存为29.9个月(13.4个月-NA),PD-L1(-)患者为18.2个月(12.7~27.2个月)。对于进展期肾癌患者包括PD-L1(+)及(-),均可从不同剂量的nivolumab治疗中获益。
关于抗PD-1通路生物标志物的选择是目前研究者更为关注的焦点。今天的口头报告中,Toni K Choueiri报道了多中心前瞻性研究(NCT01358721)的结果。非初治转移性肾癌(mRCC)患者nivolumab采用3个剂量水平:0.3 mg/kg、2 mg/kg、10mg/kg,初治患者采用10 mg/kg Q3w。基线和第2周期第8天进行肿瘤活检。56例患者进行了活检,其中32%PD-L1(+)(膜表达≥5%定义为阳性)。有效患者中(肿瘤缩小≥20%),免疫活性可以见到以下的改变:r-IFN激活的血清标志物升高,其中CXCL-9与总生存的改善显著相关(HR=0.7,95%CI 0.5-1.1);提示淋巴及髓系细胞浸润并活化免疫检测点的基因表达上调;血清TCR克隆下降;肿瘤组织中T 细胞浸润增加。在nivolumab治疗的mRCC患者中,CTLA-4(P=0.002)及PD--L2(P=0.002)显著上调。研究再次证实了PD-1单抗带来的生存获益,更为重要的是,研究发现了TCR基因表达、r-IFN相关细胞因子等有意义的相关生物学指标,有可能作为将来的生物标志物。
对于免疫治疗药物,如何选择患者是决定性的、未能回答的问题之一。免疫组化测定的PD-L1表达是目前研究较多的预测因子,尽管它在mRCC患者中的预后价值已经在某种程度上确立,但由于采用不同抗体,并且阳性节点的不同选择等使之尚无法完全作为PD-1/PD-L1单抗疗效预测指标;进一步的免疫相关标志物的研究已取得了初步结果,值得期待。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#生存获益#
37
#进展期#
0
#ASC#
27
#PD-1单抗#
37
免疫治疗不仅是肾癌,其他的肿瘤同样会获益
161