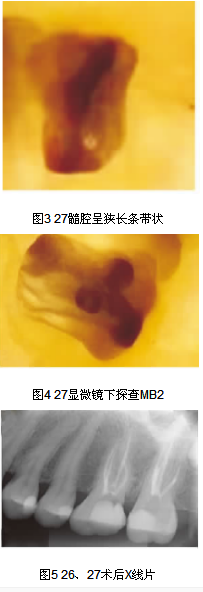
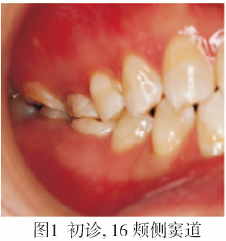
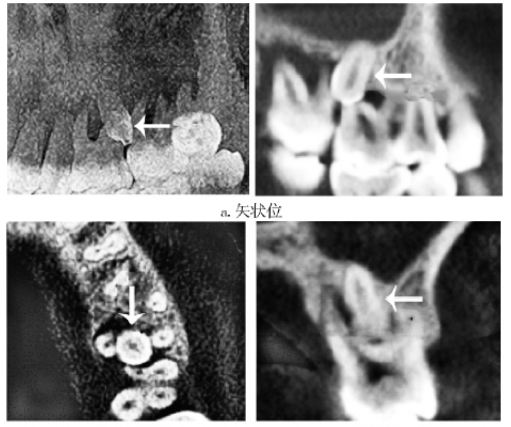
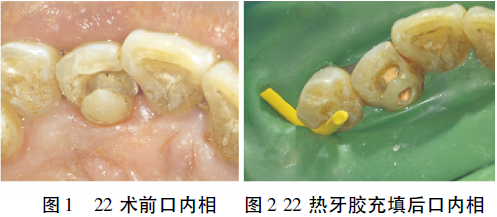
上颌第二磨牙根管上端弯曲伴MB21例
2019-12-02 朱地 刘利苹 牙体牙髓牙周病学杂志
根管弯曲,特别是根管入口处弯曲可增加根管治疗的难度。上颌第二磨牙髓室及根管系统的变异率更高,狭窄的髓室底视野较差,易导致MB2根管的遗漏,同时也增加了预备MB2的难度。1-2型MB2是根管上段为1个根管口,中下端分为两个根管,其发生率约3.7%。我们接诊了1例上颌第二磨牙根管入口急弯伴近颊根1-2型的患者,现报道如下。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#MB2#
43
#根管#
26
#磨牙#
31
#牙根#
28
#上颌#
25