BMJ:近300万人群数据揭示孕期使用阿片类药物与后代先天性畸形的关系
2021-02-12 MedSci原创 MedSci原创
在妊娠早期使用处方阿片类药物与大多数考虑的畸形类型风险无关,但会导致后代腭裂和口腔裂的风险增加。
怀孕期间发生疼痛很常见。除了通常影响育龄妇女的疼痛原因之外,孕妇还会经历一系列生理变化,包括韧带松弛和体重增加等,后者都可能诱发甚至加重一系列疼痛状况。因此,在怀孕期间,包括阿片类药物在内的镇痛药也经常被使用。
曾有研究就美国全国范围进行统计,数据表明,约22%的医疗补助受益人和14%的商业保险受益人在怀孕期间使用过至少一种阿片类处方药物。在欧洲国家、加拿大和澳大利亚,怀孕期间使用阿片类药物的频率虽然低于美国,但比例也不低(在大多数研究人群中约为5%)。

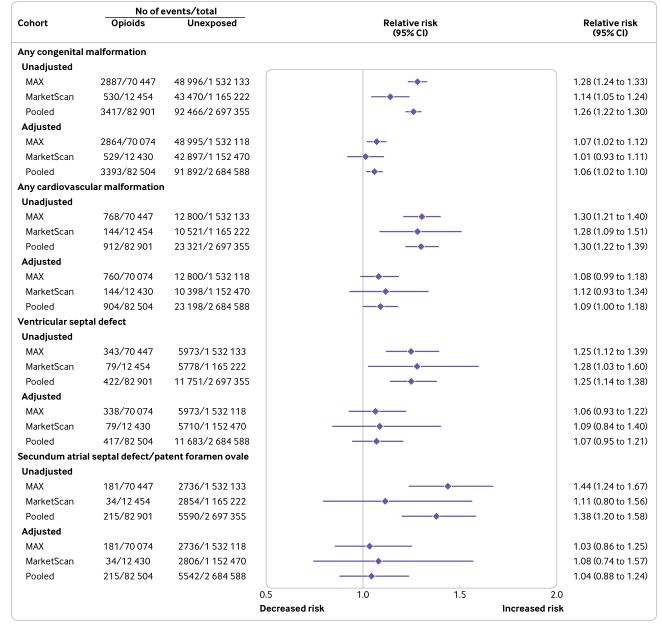
流行病学研究显示,阿片类药物可能具有致畸作用,但目前的证据仍十分有限且相互矛盾。不久前,美国疾病控制和预防中心(CDC)的一项meta分析发现,以往有关阿片类药物至畸的相关研究大多认为与先天性畸形、心血管畸形、室间隔缺损/房间隔缺损、脊柱裂、口腔裂和马蹄内翻足等疾病的总体风险增加有关。但鉴于证据的质量不高,阿片类药物与先天性畸形之间的联系仍存在相当大的不确定性。
为此,来自美国哈佛大学医学院及布莱根妇女医院的联合专家团队对妊娠早期暴露于阿片类药物妇女后代畸形风险进行了全面的评估。相关结果发表在最新的《英国医学杂志》(BMJ)上。
该研究共纳入1602580名参加社会保险和1177676名参加商业保险的孕妇。阿片类处方药物的使用标准是妊娠早期(怀孕后头3个月)要求至少使用两次阿片类药物。主要检测结果是后代心脏畸形、室间隔缺损、房间隔缺损/卵圆孔未闭、神经管缺损、马蹄内翻足和口腔裂等的畸形发生率。
结果显示,参与社会公共保险和商业保险的孕妇分别有4.4%(70447人)和1.1%(12454人)在妊娠前三个月内有两次及以上阿片类药物的使用记录。使用阿片类药物孕妇人群后代的畸形绝对风险总体上为41.0 (95%CI:39.5-42.5),而参加社会保险和商业保险妇女的总体风险分别为32.0 (31.7-32.3)与37.3 (37.0-37.7)。
进行混杂因素校正后发现,与整体孕妇人群相比,使用阿片类药物孕妇的后代腭裂和口腔裂的相对风险最高,分别为62%与21%。进一步进行分析显示,在心血管畸形、室间隔缺损、房间隔缺损/卵圆孔未闭、神经管缺损和马蹄内翻足风险虽然分别增加9%、7%、4%、5%与6%,但并没有统计学意义。
研究人员指出,阿片类药物的致畸作用在生物学上主要与内源性阿片类药物相似,后者主要参与生长发育等各个环节。因此,大家普遍认为在怀孕的关键时期使用外源性阿片可能会扰乱正常的发育过程,导致先天性畸形。
综上,该研究显示,在妊娠早期使用处方阿片类药物与大多数考虑的畸形类型风险无关,但会导致后代腭裂和口腔裂的风险增加。
参考文献:
Bateman Brian T,. et al. Association of first trimester prescription opioid use with congenital malformations in the offspring: population based cohort study BMJ 2021; 372 :n102. Doi: 10.1136/bmj.n102
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习
78
#BMJ#
25
对临床有指导价值
72
#阿片类药物#
25
#阿片类#
29
#畸形#
35
#先天性#
23
好文章!
91