Blood:Obinutuzumab、依鲁替尼和venetoclax联合靶向疗法用于慢性淋巴细胞白血病的1b期研究结果
2018-08-17 MedSci MedSci原创
现已证实包含抗CD20单克隆抗体obinutuzumab、Bruton酪氨酸激酶抑制剂依鲁替尼和Bcl2抑制剂venetoclax的靶向疗法用于慢性淋巴细胞白血病(CLL)患者具有显著的临床疗效,表明基于互补机制的联合疗法是理想的。但是,将venetoclax与其他活性药物联合使用会增加肿瘤溶解综合征的风险,阻碍了该种联合方案的临床推广。Kerry A. Rogers等研究人员为将这种风险降至最低
Kerry A. Rogers等研究人员为将这种风险降至最低,设计并实施了一种持续固定的方案,即依次给药:obinutuzumab→依鲁替尼(第2个疗程)→venetoclax(第3个疗程),一共14个疗程(28天一疗程)。本研究共招募了12位复发性/难治性CLL患者,均采用研究方案进行治疗。研究人员还检测了venetoclax的剂量水平,并鉴定了FDA批准的三种药物剂量以供联合应用。
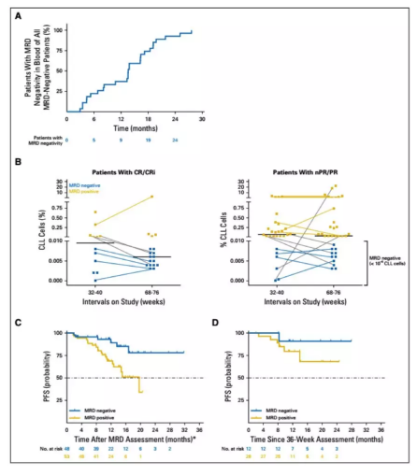
治疗过程中所出现的副反应与已知的单药毒副作用一致,其中血液方面的不良反应最常见,未发生明显的肿瘤溶解综合征。总体缓解率高达92%(95% CI 62-100%),其中42%(5/12)的患者获得完全缓解或完全缓解伴骨髓部分恢复。在治疗结束后,有6位患者的血液和骨髓中均检测不到CLL残留。
综上所述,本研究表明这种方案用于CLL患者可有效诱导深度缓解,并且安全性高,为进一步开展2期乃至3期临床试验提供了依据。
Kerry A. Rogers,et al. Phase. 1b study of obinutuzumab, ibrutinib, and venetoclax in relapsed and refractory chronic lymphocytic leukemia. Blood 2018 :blood-2018-05-853564; doi: https://doi.org/10.1182/blood-2018-05-853564
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#mAb#
38
#联合靶向#
33
#NET#
37
#研究结果#
30
#淋巴细胞白血病#
33
#淋巴细胞#
31
#靶向疗法#
56
#Obinutuzumab#
48