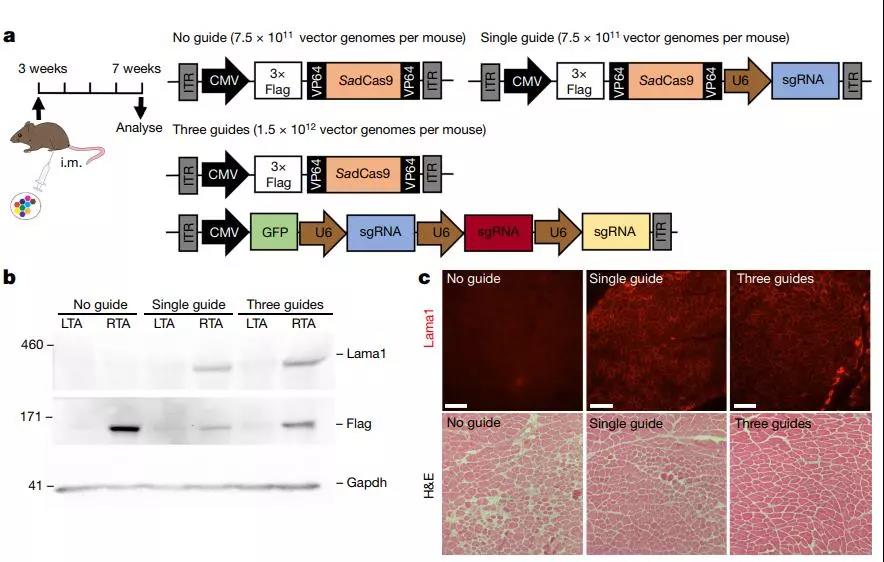
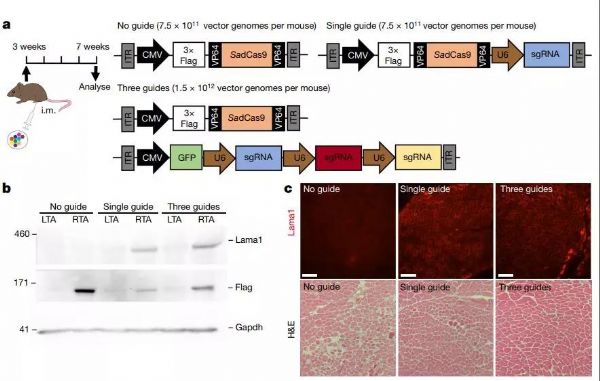
Nature:肌营养不良可咋整?CRISPR带来治疗新曙光
2019-07-31 苏煜静 生物探索
肌营养不良是一种遗传性肌肉消耗疾病,临床表现为不同程度的骨骼肌肉萎缩,严重时甚至累及心肌。据不完全统计,全球大约每3600个男孩中就有一个患有这种疾病,一般患者的寿命只有二十多岁。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肌营养不良#
25
#Nat#
27
#曙光#
33
#CRISPR#
30
向科研人员致敬!!!
73