Cell Death Differ:PP2Acα促进巨噬细胞积累加剧肾脏纤维化的发生
2021-05-03 xiaozeng MedSci原创
慢性肾病(CKD)一般表现为肾小球滤过率降低、尿白蛋白排泄增加或两者兼具,该疾病正成为日益严重的公共卫生问题。
慢性肾病(CKD)一般表现为肾小球滤过率降低、尿白蛋白排泄增加或两者兼具,该疾病正成为日益严重的公共卫生问题。无论CKD的最初病因为何,间质纤维化是其共同的病理特征,且与CKD患者的长期预后高度相关。
既往研究显示,包括炎症反应、成纤维细胞活化、肾小管萎缩和微血管稀疏在内的多种事件均会导致肾间质纤维化。作为炎症反应的主要介质,巨噬细胞的积累已被证实高度参与肾脏损伤和修复的过程。然而,其潜在的机制尚不清楚。
在该研究中,研究人员通过分析患有肾纤维化的患者和动物模型的肾脏组织,发现巨噬细胞中PP2Acα大量表达。通过构建可诱导性巨噬细胞PP2Acα敲除小鼠模型。相比于同窝对照组,单侧输尿管阻塞或缺血再灌注损伤后,PP2Acα基因敲除小鼠较少出现肾纤维化、巨噬细胞的蓄积或肾小管细胞的死亡。
在纤维化肾脏巨噬细胞中PP2Acα的表达上调
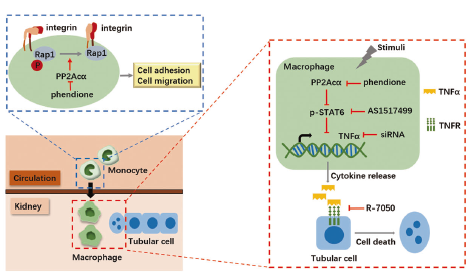
在培养的巨噬细胞中,缺乏PP2Acα会通过抑制Rap1活性进而导致细胞运动性的降低。此外,共培养PP2Acα-/-巨噬细胞与肾小管细胞则表现出较少的肾小管细胞死亡,这归因于巨噬细胞中Stat6介导的TNFα(肿瘤坏死因子α)生成的减少。
相关模型示意图
总而言之,该研究揭示PP2Acα能够促进巨噬细胞的积累和激活,并通过调节Rap1的激活和TNFα的产生来加速肾小管细胞死亡和肾脏纤维化的发生。
原始出处:
Liang, Y., Sun, X., Wang, M. et al. PP2Acα promotes macrophage accumulation and activation to exacerbate tubular cell death and kidney fibrosis through activating Rap1 and TNFα production. Cell Death Differ (01 May 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Cell#
26
#CEL#
22
#Differ#
37
#Death#
39