AHA2019丨STEMI患者的非罪犯血管斑块形态:COMPLETE试验OCT亚组研究结果
2019-11-18 国际循环编辑部 国际循环
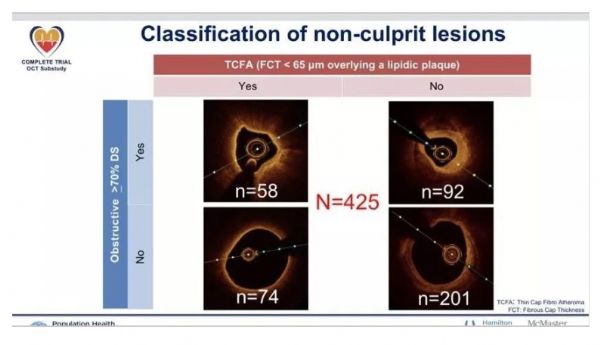
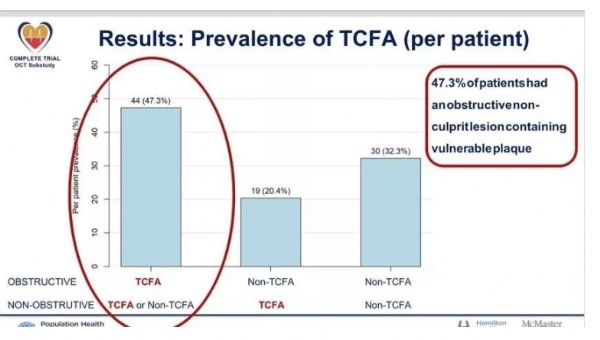
11月17日,在2019美国心脏协会科学年会(AHA 2019)上,来自美国人口健康研究协会、McMaster大学和汉密尔顿健康科学研究所的Natalia Pinilla-Echeverri教授发表主题报告,阐述ST段抬高型心肌梗死(STEMI)患者的非罪犯血管斑块形态的OCT特点。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#OCT#
37
#非罪犯血管#
28
#MPL#
35
#研究结果#
30
#complete#
33
#STEMI患者#
39
#AHA#
23
#斑块#
26
#STEM#
35