J Clin Oncol:放疗(RT)和雄激素剥夺疗法(ADT)联合或不联合多西他赛治疗非转移性的不良风险前列腺癌的疗效:一项前瞻性随机研究
2021-07-03 yd2015 MedSci原创
对于非转移性的不良风险前列腺癌患者,在放疗(RT)和雄激素剥夺疗法(ADT)的基础上加入多西他赛并不能延长OS。
在两项随机对照试验(RCT)中观察到总体生存期(OS)获益后,多西他赛(Docetaxel)首次被美国食品和药物管理局(FDA)批准用于男性转移性(M1)去势抵抗的前列腺癌(PC)患者。随后,在两项RCT中,当多西他赛加入雄激素剥夺治疗(ADT)时,在新诊断的M1去势敏感PC患者中观察到较长的OS。随后,在7个随机对照试验中,研究了对不良风险非转移性(M0)前列腺癌的男性,加用多西他赛到根治性前列腺切除术(RP)或放疗(RT)和ADT的疗效; 到目前为止,有6项研究报告为阴性或不确定的结果。其中6例研究性的2项研究中(>80%患者为高级别),可以观察到前列腺癌特异性死亡(PCSM)的降低,有OS的获益倾向。因此,国外学者开展了前瞻性研究,评估多西他赛联合雄激素剥夺治疗(ADT)+ 放疗(RT)对新诊断的男性非转移性伴有不良风险的前列腺癌患者的疗效。相关结果发表在Journal of Clinical Oncology杂志上。

该研究(NCT00116142)是研究者发起的多中心随机研究。主要研究终点为OS,放疗(RT)导致的肿瘤发生率和前列腺特异性抗原(PSA)分层(<4, >20 v 4-20ng/mL)评估OS获益情况。2005年9月21日至2015年1月13日, 350例男性分期T1c-4N0M0伴有不良风险的前列腺癌(PC)患者,随机分配(1:1)接受放疗(RT)和雄激素剥夺疗法(ADT) +多西他赛(60mg/ m 2/3周共三周期在RT前和RT期间20mg/ m 2/1周)和ADT+RT。两组各有175例患者。
中位随访时间为10.2年(8.00-11.40年)。多西他赛组和ADT+RT组的10年OS率分别为72% (95% CI 63to79)和74%(95% CI 66to 80)(HR=0.99, 95% CI 0.65 to 1.51, P=0.98)。而多西他赛的加入降低的RT导致的第二肿瘤的发生和相关死亡(年龄调整HR=0.13,95% CI, 0.02 to 0.97; P =0.046)。评估的10年累计发病率分别为0.61% (95% CI 0.06 to 3.09)和4.90% (95% CI 2.13 to 9.40)。但是所有的第二原发肿瘤是没有区别的(HR=0.89, 95% CI 0.50 to 1.60; P=0.70)。

疗效评估
对于PSA<4 ng/mL对比4-20 ng/mL的患者,多西他赛对OS的治疗效果不同(HR, 0.33, 1.40;P interaction=0.09与年龄调整HR, 0.27,1.51,P interaction <0.05),可能是在PSA<4 ng/mL的患者中,因为多西他赛组导致更低的PCSM,(0 / 13 [0.00%]v 4 / 14[28.57%])。
对于PSA>20 ng/mL对比4-20 ng/mL的患者,多西他赛对OS的治疗效果同样不同(HR, 0.62, 1.40; P interaction=0.08与年龄调整HR, 0.60, 1.51; P interaction<0.05),但是这次不能解析为多西他赛组导致更低的PCSM,因为多西他赛和ADT+RT组的PCSM分别为10 of 49(20.41%)和8 of 45(17.78%)。
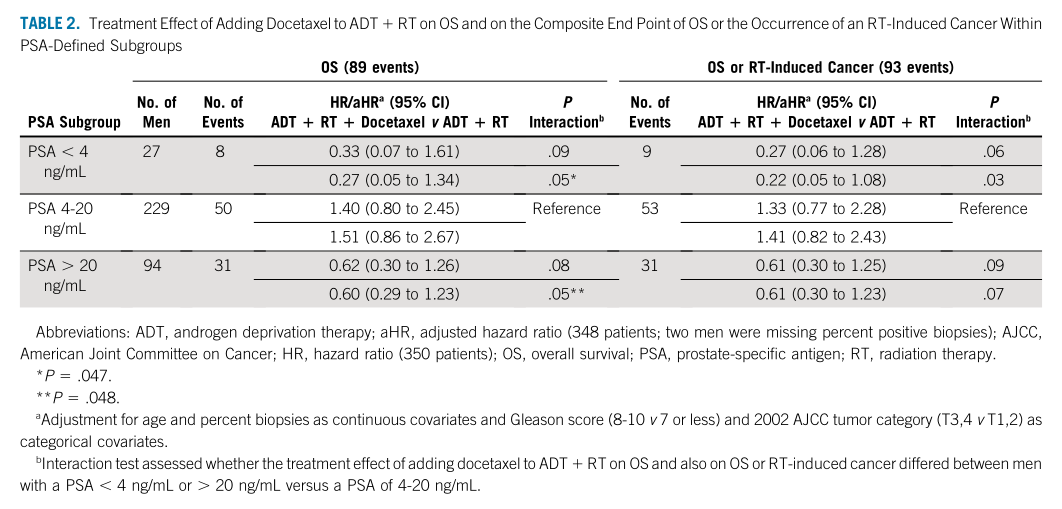
PSA分层评估OS
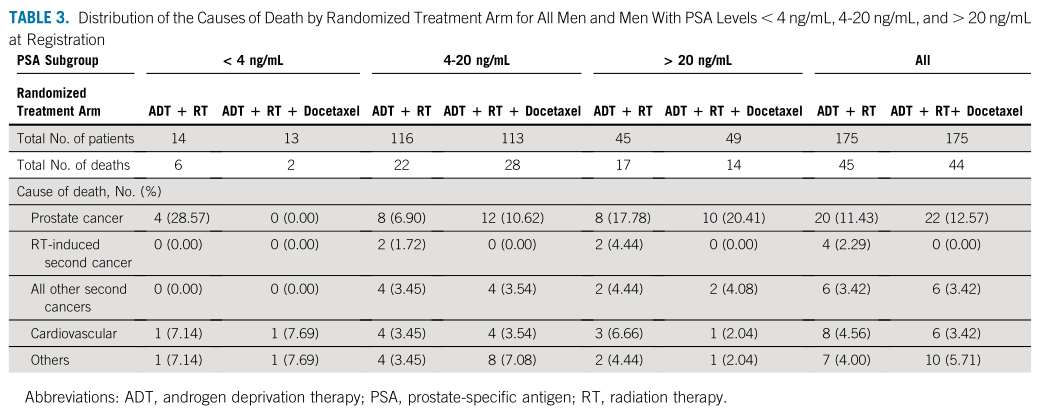
PSA分层死亡分布
多西他赛组和ADT+RT组的中断治疗比例分别为4.09%和4.60%。两组严重的急性不良事件分别为26.90%和10.34%。两组2/3级不良事件分别为18.13%和8.05%。4级不良事件为8.77%和1.72%。ADT+RT组有1例5级不良事件(突然死亡),但是不确定为治疗相关。严重的迟发不良事件分别为81.87%和73.56%。大多数为1/2级,分别为67.25%和63.22%;3/4级分别为14.62%和10.34%。
综上,对于非转移性的不良风险前列腺癌患者,在放疗(RT)和雄激素剥夺疗法(ADT)的基础上加入多西他赛并不能延长OS。但是可以降低RT导致的第二原发肿瘤的发生率,以及在PSA , 4 ng/mL的患者中,可以通过降低前列腺癌特异性死亡(PCSM)来延长OS。
原始出处:
D'Amico AV, Xie W, McMahon E, et al. Radiation and Androgen Deprivation Therapy With or Without Docetaxel in the Management of Nonmetastatic Unfavorable-Risk Prostate Cancer: A Prospective Randomized Trial. J Clin Oncol. 2021 Jul 1:JCO2100596. doi: 10.1200/JCO.21.00596. Epub ahead of print. PMID: 34197181.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#前瞻性#
24
#随机研究#
32
#非转移#
33
#非转移性#
28
#雄激素剥夺#
19
#Oncol#
16
#转移性#
25
#ADT#
38
谢谢梅斯提供这么好的信息,学到很多
46
谢谢梅斯分享这么多精彩信息
39