Ann Hematol:在卡帕珠单抗前时代获得性血栓性血小板减少性紫癜的死亡率
2021-12-31 MedSci原创 MedSci原创
首次出现 aTTP 的患者在诊断时昏迷或昏迷以及第 6 天对 PEX 缺乏反应是死亡率的强预测因子。
获得性血栓性血小板减少性紫癜(aTTP)是由ADAMTS13金属蛋白酶的免疫介导的防御引起的,随后血管内皮表面的超大血管性血肿因子多聚体持续存在,血小板聚集增加。尽管血浆置换 (PEX) 和免疫抑制剂在治疗 aTTP 方面有效,但仍有许多患者死于该病。对这些患者的早期识别是至关重要的,因为他们可以受益于新兴药物,如卡普西珠单抗,一种抗血管性血友病(vW)纳米体,可以阻止血小板聚集到小血管中,但卡普西珠单抗是否可以挽救这些患者仍然悬而未决。
本次研究的目的是表征 aTTP 第一次发作的死亡率模式和预后因素,旨在早期识别aTTP首发时死亡高危患者,特别关注现成的临床数据,由此病人可以从新的治疗方法中获益。
研究者在西班牙 TTP 登记处查询了在就诊发作中被诊断为 aTTP 且满足完整临床和随访数据的患者(n = 102)。这些患者是在 2004 年至 2018 年间确诊的,并且都接受了每日 PEX 和皮质类固醇治疗。在诊断和治疗过程中分析临床和实验室数据。
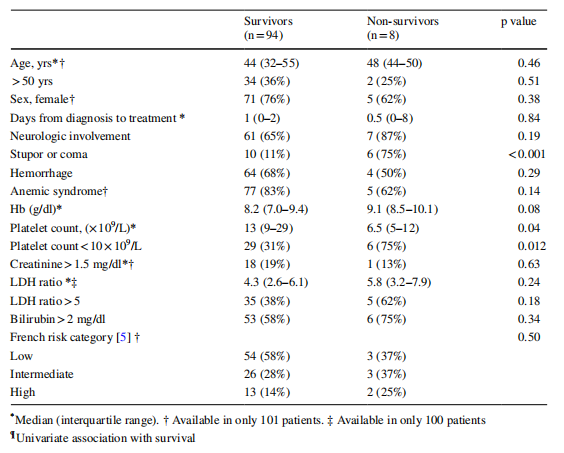
表1:获得性血栓性血小板减少性紫癜的临床资料
8 名患者 (7.7%) 在就诊后 12 小时至 36 天之间死亡,可分为三种模式:治疗前死亡、急性心脏或神经系统事件导致的早期死亡以及未缓解的 aTTP 导致的晚期死亡。诊断时昏迷或昏迷和治疗第 6 天时血小板计数 < 20 × 10 9 /L 与死亡风险增加独立相关。
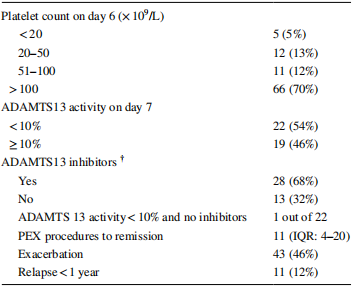
表2:8例非存活患者的临床特征
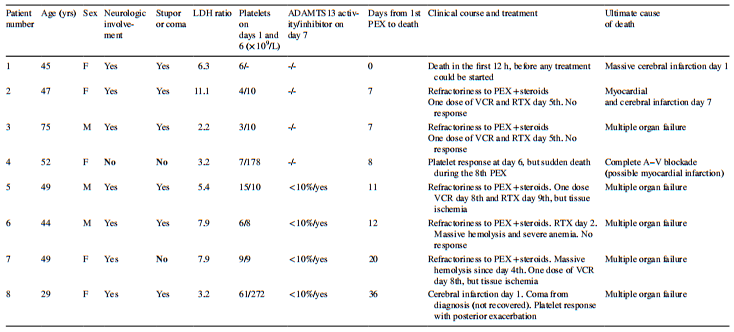
表3:94例aTTP前期存活患者的随访特征
在本研究中,与aTTP首次发作相关的总死亡率为8%。在治疗第6天,严重意识下降和未能达到血小板反应的患者的死亡率增加。相反,在诊断时没有意识下降和血小板对治疗反应迅速的患者在PEX和免疫抑制剂下表现非常好,尽管其中一些患者后来出现了短暂的疾病恶化。

图1:102例自身免疫性血栓性血小板减少性紫癜首次发作患者的死亡率预后因素的ROC曲线分析。诊断时评估昏迷;除2例较早死亡的患者外,在第6天评估血小板计数。AUC:曲线下的面积。PPV:阳性预测值。NPV:负预测值
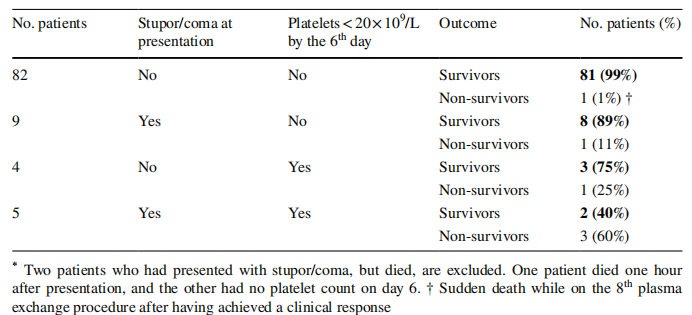
表4:100例获得性血栓性血小板减少性紫癜的结局。两名出现昏迷但死亡的患者被排除在外。一名患者在就诊后1小时死亡,另一名患者在第6天无血小板计数。†在第8次血浆置换手术中获得临床反应后猝死
严重的意识抑制已经被确定为是aTTP的不良预后标志,预示着治疗的顽固性和持续性疾病导致的死亡。在研究中,16例强化PEX患者中有10例出现昏迷,从而强调了早期诊断和治疗aTTP的重要性。
这项研究的主要优势在于患者系列的同质性:所有病例均为aTTP的频繁发作,诊断ADAMTS13活性缺失存在抗ADAMTS13抗体,并接受了相同的PEX和皮质激素前期治疗。主要的局限性是事件的数量相对较少,这可能妨碍了对attp驱动的死亡率模式进行更全面的分析。
总的来说,诊断时无麻木或昏迷,且血小板对PEX反应快,是首发aTTP患者最常见的模式,预后良好。相比之下,PEX和免疫抑制剂难以治疗的严重意识抑郁和持续性血小板减少症并不常见,但预后不良。后者患者是评价卡普单抗等新型药物对早期抑制微血管血栓形成的挽救潜力的试金石。
原始出处:
del Río-Garma, J., Bobillo, S., de la Rubia, J. et al. Mortality in acquired thrombotic thrombocytopenic purpura in the pre-caplacizumab era. Ann Hematol (2021). https://doi.org/10.1007/s00277-021-04685-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血小板减少性紫癜#
34
#获得性#
47
#血栓性#
36
#血小板减少#
41
#EMA#
33
#紫癜#
29
#血栓性血小板减少性紫癜#
39