Br J Dermatol:化脓性汗腺炎中一个独特的促炎因子——IL-36
2017-11-02 MedSci MedSci原创
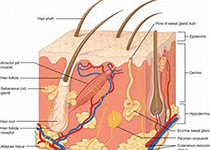
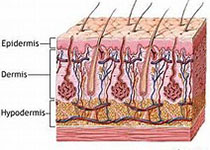
背景:白细胞介素(IL)- 36家族可能参与炎症性疾病的治疗。大汗腺感染后在皮内和皮下组织反复发作,广泛蔓延,形成范围较广的慢性炎症、小脓肿、复杂性窦道和瘘管,称为化脓性汗腺炎(suppurative hidrosadenitis)。发病部位多在大汗腺分布区,如腑下、肛门、生殖器、臀部、股部、腹股沟、乳晕、脐部和外耳道,发生于肛门周围者称为肛周化脓性汗腺炎。在中医学中属蜂窝漏、串臀瘘的范畴。20~
背景:白细胞介素(IL)- 36家族可能参与炎症性疾病的治疗。大汗腺感染后在皮内和皮下组织反复发作,广泛蔓延,形成范围较广的慢性炎症、小脓肿、复杂性窦道和瘘管,称为化脓性汗腺炎(suppurative hidrosadenitis)。发病部位多在大汗腺分布区,如腑下、肛门、生殖器、臀部、股部、腹股沟、乳晕、脐部和外耳道,发生于肛门周围者称为肛周化脓性汗腺炎。在中医学中属蜂窝漏、串臀瘘的范畴。20~40岁身体肥胖多汗的人,易患此病,女多于男。目标:本研究旨在分析化脓性汗腺炎(HS)患者的皮肤中,IL-36α、β、γ和其拮抗细胞因子的表达IL-36α、IL-37、IL-38的表达情况。方法:研究人员收集了皮损部位的皮肤样本和相应的HS病灶周围皮肤的皮肤样本,以及健康对照组患者的皮肤样本,并通过实时定量RT-PCR对它们进行了分析。研究人员通过对一个皮肤样本子集的免疫组化研究来评价IL-36α、β和γ的PCR情况。结果:与健康对照组相比,HS患者皮损皮肤处的IL-36α、β、γ的表达水平均显著较高。与健康对照组相比,HS病灶周围皮肤中的IL-37和IL-38明显较高,但二者在HS皮损皮肤中表
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#促炎#
35
#促炎因子#
47
#化脓性#
29
签到学习了--
74
签到学习了--
72
签到学习了--
75
签到学习了--
76
签到学习了--
69
签到学习了--
25
签到学习了--
19