Prostate Cancer P D:前列腺癌中质子放射治疗与光子放射治疗比较
2019-04-23 AlexYang MedSci原创
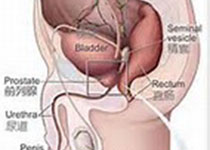
放射技术的进展改变了局部前列腺癌患者的治疗选择。三维适形放射治疗和可调节强度放射治疗(IMRT)使得医生可以避免邻近正常组织受放射影响,从而减少副作用事件。质子束技术的引入及其在病理组织中能量具有最大范围的物理优势,有可能为前列腺癌患者避免膀胱和直肠等关键器官遭受影响。目前的数据局限于大的和观察性的研究,并且并没有阐释清楚质子治疗比IMRT传统治疗方法的优势。另外,质子束放射治疗的花费也增加了该治
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Prostate Ca#
24
#ROS#
21
#PRO#
24
#治疗比较#
33
前列腺癌相关研究,学习了,谢谢梅斯
48