Diabetologia:艾塞那肽注射液PB-119可有效治疗未治疗过的2型糖尿病
2021-03-10 MedSci原创 MedSci原创
胰高血糖素样肽1受体激动剂,如艾塞那肽,可作为维持2型糖尿病患者血糖控制的单一疗法和附加疗法。PB-119,是一种聚乙二醇化的艾塞那肽注射液,治疗2型糖尿病的疗效如何?
胰高血糖素样肽1受体激动剂(GLP-1RA),如艾塞那肽(Exenatide),可作为维持2型糖尿病患者血糖控制的单一疗法和附加疗法。PB-119,是一种聚乙二醇化的艾塞那肽注射液。
本研究调查了每周一次PB-119用于未治疗过的2型糖尿病患者的安全性和有效性。
这是一项随机、安慰剂为对照、双盲2期研究,将未治疗过的中国2型糖尿病患者按1:1:1:1随机分至四组,分别接受皮下安慰剂或三种皮下剂量的PB-119(75、150和200gμg)中的一种,为期12周。主要终点是糖化血红蛋白(HbA1c)的变化,其他终点有空腹血糖、餐后2小时血糖,以及治疗第2、4、8和12周时HbA1c<53 mmol/mol(<7.0%)和≤为48 mmol/mol(≤6.5%)的患者比例。
HbA1c随治疗的变化
共251位患者被随机分为4个治疗组(安慰剂组 n=62例、PB-119 75 μg组、150 μg组和200 μg组各63例)。治疗12周后,与安慰剂组相比,75μg组、150 μg组和200 μg组的经基线HbA1c校正后的HbA1c平均差值分别为-7.76 mol/mol(-0.72%)、-12.89 mmol/mol(-1.18%)和-11.14 mmol/mol(-1.02%),所有p值均<0.001。
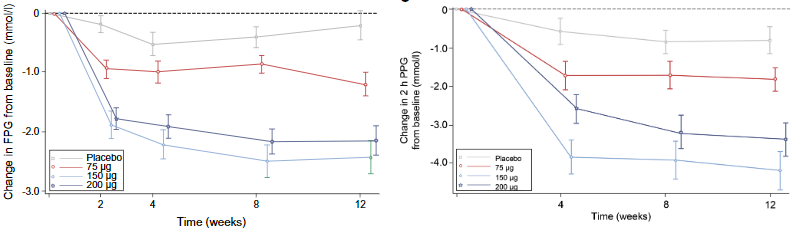
FPG和PPG的变化
在不同时间点的其他疗效终点也观察到了类似的结果。
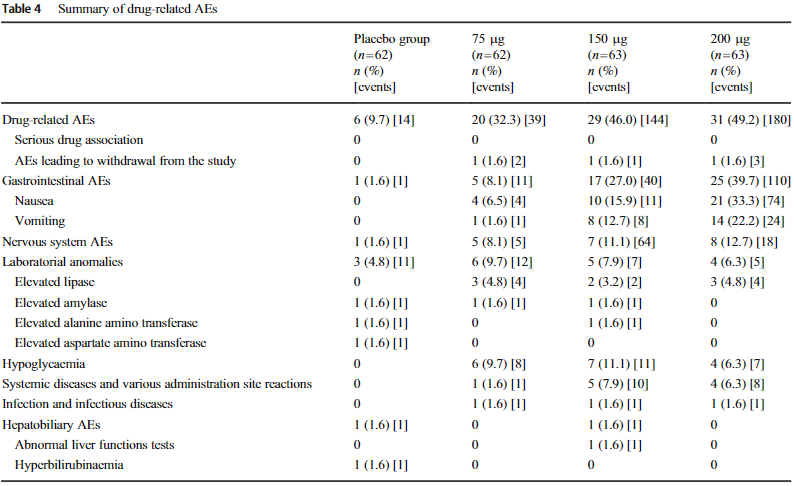
药物相关不良事件
未发生需紧急治疗的严重不良事件、严重低血糖和死亡。
综上,与安慰剂相比,所有测试的PB-119剂量用于既往未治疗过的中国2型糖尿病患者12周内都具有更好的疗效,而且安全性和耐受性良好。
原始出处:
Ji Linong,Du Ying,Xu Min et al. Efficacy and safety of PEGylated exenatide injection (PB-119) in treatment-naive type 2 diabetes mellitus patients: a Phase II randomised, double-blind, parallel, placebo-controlled study. Diabetologia, 2021, 10.1007/s00125-021-05392-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#BET#
29
太好了
61
#DIA#
39
#艾塞那肽#
49
#注射液#
48
#有效治疗#
31
认真学习了
78
谢谢MedSci提供最新的资讯
61
好文章!
79