Int J Cardiol:新型降糖药物的心血管预后分析!
2017-12-21 xing.T MedSci原创
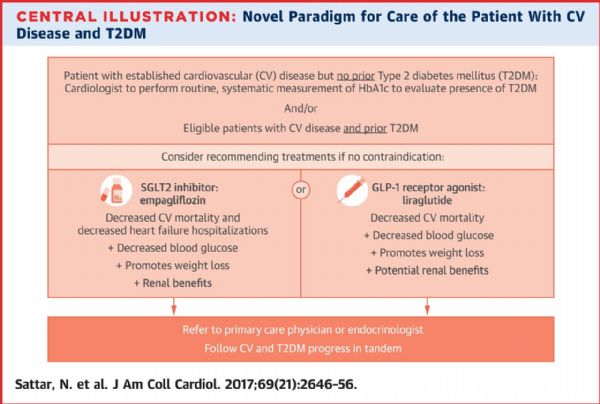
由此可见,SGLT-2抑制剂和GLP-1 Ras可降低全因死亡率和MACE,但是DPP-4抑制剂无此效应。SGLT-2抑制剂对全因死亡率的影响最大。DPP-4抑制剂没有展示出具有心血管益处,并且在预防死亡方面不如其他两种药物。
直接比较新型降糖药物心血管预后的随机对照试验(RCTs)较为缺乏。近日,心血管领域权威杂志International Journal of Cardiology上发表了一篇研究文章,研究人员采用网络荟萃分析来比较不同新型降糖药物类别的主要不良心血管事件(MACE)和死亡率。
研究人员检索了MEDLINE、EMBASE、Cochrane数据库和ClinicalTrials.gov,检索时间截止至2016年12月30日,纳入了研究对象为服用SGLT-2抑制剂、胰高血糖素样肽-1受体激动剂(GLP-1 RAs)和二肽基肽酶-4(DPP-4)抑制剂的糖尿病患者并报告MACE和死亡的研究。研究人员使用R统计量对频率和贝叶斯方法进行结局比较。
该网络荟萃分析纳入了包含有62268名患者的7项随机对照试验。SGLT-2抑制剂和GLP-1 RA抑制剂相比于安慰剂可以显著降低MACE(分别有0.85,95%可信区间为0.73-0.99和0.89, 95%可信区间为0.82-0.97)和全因死亡率(分别为0.67, 95%可信区间为0.55-0.81和0.89, 95%可信区间为0.80-0.99)。此外,与GLP-1 RA相比,SGLT-2抑制剂可降低全因死亡率(0.76,0.61-0.94)。相比之下,与安慰剂相比,DPP-4抑制剂并不能降低MACE或死亡率,并且与SGLT-2抑制剂(1.53,1.24-1.89)和GLP-1RA(1.16,1.01-1.33)相比,DPP-4抑制剂与更高的全因死亡率相关。
由此可见,SGLT-2抑制剂和GLP-1 Ras可降低全因死亡率和MACE,但是DPP-4抑制剂无此效应。SGLT-2抑制剂对全因死亡率的影响最大。DPP-4抑制剂没有展示出具有心血管益处,并且在预防死亡方面不如其他两种药物。
原始出处:
Yue Fei,et al. Network meta-analysis of cardiovascular outcomes in randomized controlled trials of new antidiabetic drugs.International Journal of Cardiology.2017.http://www.sciencedirect.com/science/article/pii/S0167527317311427
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cardiol#
41
如此说来还是一个好事情
72
#降糖药#
36
#降糖药物#
41
#心血管预后#
42
学习了.谢谢.
70
xuex
66
henhao
76