mBio:儿童社区获得性肺炎短疗程与标准疗程抗生素治疗的效果比较
2022-03-31 小文子 MedSci原创
抗生素使用可能破坏微生物菌群并导致抗菌治疗后的不良事件,该研究为减少抗生素使用提供了依据。
儿童社区获得性肺炎(CAP)通常需要抗生素治疗10天。缩短抗生素疗程的治疗策略已被提出作为降低抗生素耐药的策略。美国微生物学会(ASM)发表在mBio杂志的一项研究评估了接受短期和标准抗生素治疗疗程的CAP患者的微生物组(抗生素耐药性和微生物群)变化。
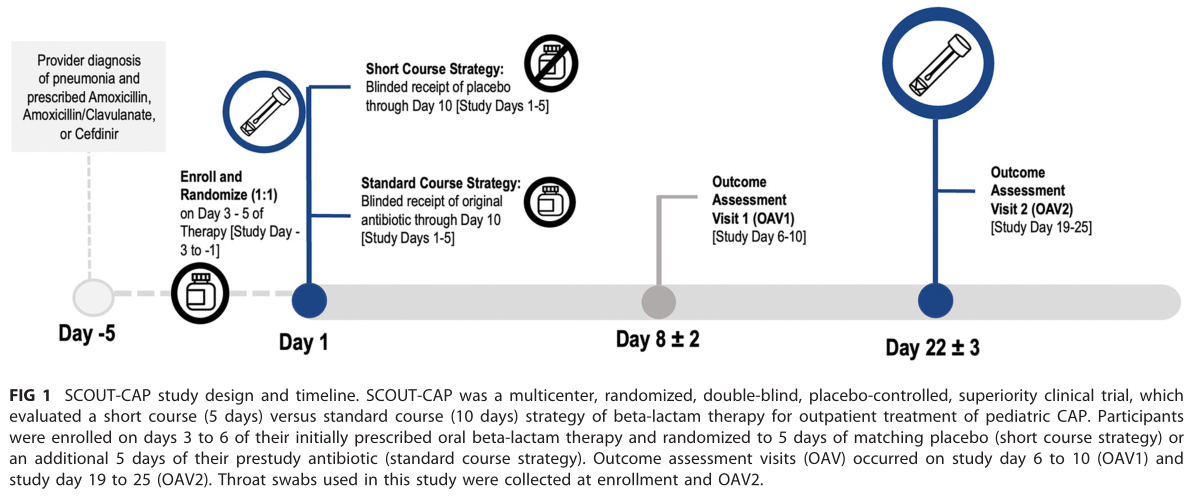
数据来自SCOUT-CAP试验的6~71个月龄儿童(n = 171)。CAP患者随机接受短期(5天)与标准(10天)β-内酰胺治疗策略。在入组和研究结束时收集咽拭子。91%的参与者最初使用的抗生素是阿莫西林,然后是阿莫西林/克拉维酸钾(6%)和头孢地尼(2%)。短疗程组和标准策略组在年龄、性别、种族、民族或初始抗生素处方方面无差异。
研究结果
1.呼吸道抗生素抗性基因(ARGs)丰度和多样性
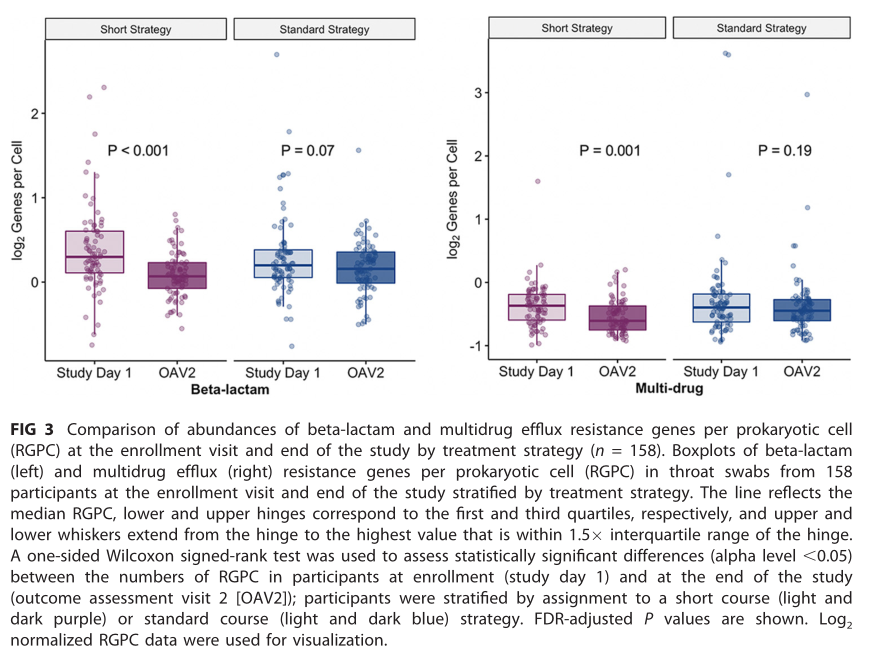
研究结束时,短疗程和标准疗程组原核细胞β-内酰胺类抗生素抗性基因(RGPC)的中位丰度分别为0.55(范围0.18~1.24)和0.60(范围0.21~2.45)。
β-内酰胺RGPC的Wilcoxon效应量较小(r=0.15;95% CI,0.01~0.29)。短疗程儿童大环内酯类RGPC和多重耐药泵ARGs显著低于标准疗程组(P=0.05),大环内酯类RGPC的Wilcoxon效应量较小(r=0.15;95%CI,0.02~0.29),多重耐药泵ARG的Wilcoxon效应量中等(r=0.23;95%CI,0.09~0.37)。
2.呼吸道微生物群的分类特征
接受标准疗程的儿童微黄奈瑟球菌等的相对丰度较高,接受短程策略的儿童普雷沃氏菌属和小韦荣氏球菌的相对丰度较高。
结果显示,接受5天β-内酰胺治疗的CAP儿童ARGs显著低于接受标准10天治疗的儿童。这些数据为减少抗生素使用提供了额外依据,抗生素使用可能破坏微生物菌群并导致抗菌治疗后的不良事件。越来越多的研究验证了抗生素治疗时间较短对一系列疾病的疗效。未来抗菌药疗效和持续时间的研究应考虑对微生物群和耐药性的影响。
原文出处:
M. M. Pettigrew, J. Kwon, et al, Comparison of the Respiratory Resistomes and Microbiota in Children Receiving Short versus Standard Course Treatment for Community-Acquired Pneumonia, mBio, 2022, DOI: 10.1128/mbio.00195-22.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#获得性#
34
#Bio#
36
#抗生素治疗#
41
#社区#
43