Circulation:透析治疗的终末期肾病患者预防性植入ICD的效益和风险
2019-06-07 QQ MedSci原创
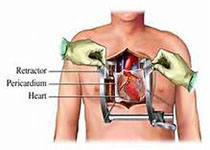
据报道,透析治疗的终末期肾病患者具有很高的心脏性猝死(SCD)风险;迄今为止,尚无有效的治疗方法来降低这一风险。预防性植入性心律转复除颤器(ICD)预防SCD的可行性和价值尚不明确。研究人员开展一个关于透析患者植入性心律转复除颤器的前瞻性、随机对照试验,在左室射血分数≥35%的透析患者中评估ICD植入预防SCD的价值和安全性。主要结点是SCD,次要结点是全因死亡率和ICD相关并发症。在纳入188例
研究人员开展一个关于透析患者植入性心律转复除颤器的前瞻性、随机对照试验,在左室射血分数≥35%的透析患者中评估ICD植入预防SCD的价值和安全性。主要结点是SCD,次要结点是全因死亡率和ICD相关并发症。
在纳入188例患者(ICD组97例、对照组91例)后,因无效原因停止试验。中位随访6.8年(四分位间距 3.8-8.8年)。共发生19例SCD(10.1%),其中11位在ICD组、8位在对照组。ICD组和对照组的5年SCD累计发病率分别为9.7%(95% CI 3.3%-16.2%)和 7.9% (95% CI, 1.7–14.0%),风险比为1.32(95% CI, 0.53–3.29; P=0.55) 。总体上,共有99位患者死亡(52.7%),ICD组52例,对照组47例。ICD组和对照组的5年存活概率分别为50.6% (95% CI, 39.8%–61.5%) 和54.5% (95% CI, 43.0–66.0%),风险比为1.02 (95% CI, 0.69–1.52; P=0.92)。ICD组接受ICD的80位患者中,发生了25例与ICD植入相关的副反应。
综上所述,透析治疗的终末期肾病患者预防性植入ICD治疗并不能降低其SCD或全因死亡率。
J. Wouter Jukema,et al. Prophylactic Use of Implantable Cardioverter-Defibrillators in the Prevention of Sudden Cardiac Death in Dialysis Patients. 4 Jun 2019https://doi.org/10.1161/CIRCULATIONAHA.119.039818Circulation. 2019;139:2628–2638
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#终末期#
29
#肾病患者#
32
#ICD#
40
#预防性#
35
#终末期肾病#
32
#植入#
22