Br J Cancer:sapanisertib治疗晚期实体瘤
2020-09-15 QQY MedSci原创
PI3K/AKT/mTOR信号转导通路参与调节细胞生长、增殖和存活。 在人癌症中经常能观察到异常的PI3K/AKT/mTOR信号。抑制mTOR会减少蛋白质的翻译并预防异常细胞的增殖和肿瘤血管生成作用。
PI3K/AKT/mTOR信号转导通路参与调节细胞生长、增殖和存活。 在人癌症中经常能观察到异常的PI3K/AKT/mTOR信号。抑制mTOR会减少蛋白质的翻译并预防异常细胞的增殖和肿瘤血管生成作用。
Sapanisertib是一种高选择性的mTOR激酶抑制剂,其可以同时抑制mTORC1和mTORC2。 该1期剂量递增/扩展研究主要评估晚期实体瘤患者口服sapanisertib的安全性和耐受性。
受试患者分为四组进行sapanisertib剂量递增给药,给药方案如下,每日一次(QD,31位患者);每周一次(QW,30位患者);吃三天停4天(QD×3dQW,33位患者);吃5天停2天(QD×5dQW,22例患者)。在扩展队列中,患肾细胞癌(RCC)、子宫内膜癌或膀胱癌的共82位患者接受5mg QD(39位)、40μmg QW(26位)或30μmg QW(17位)的sapanisertib给药治疗。
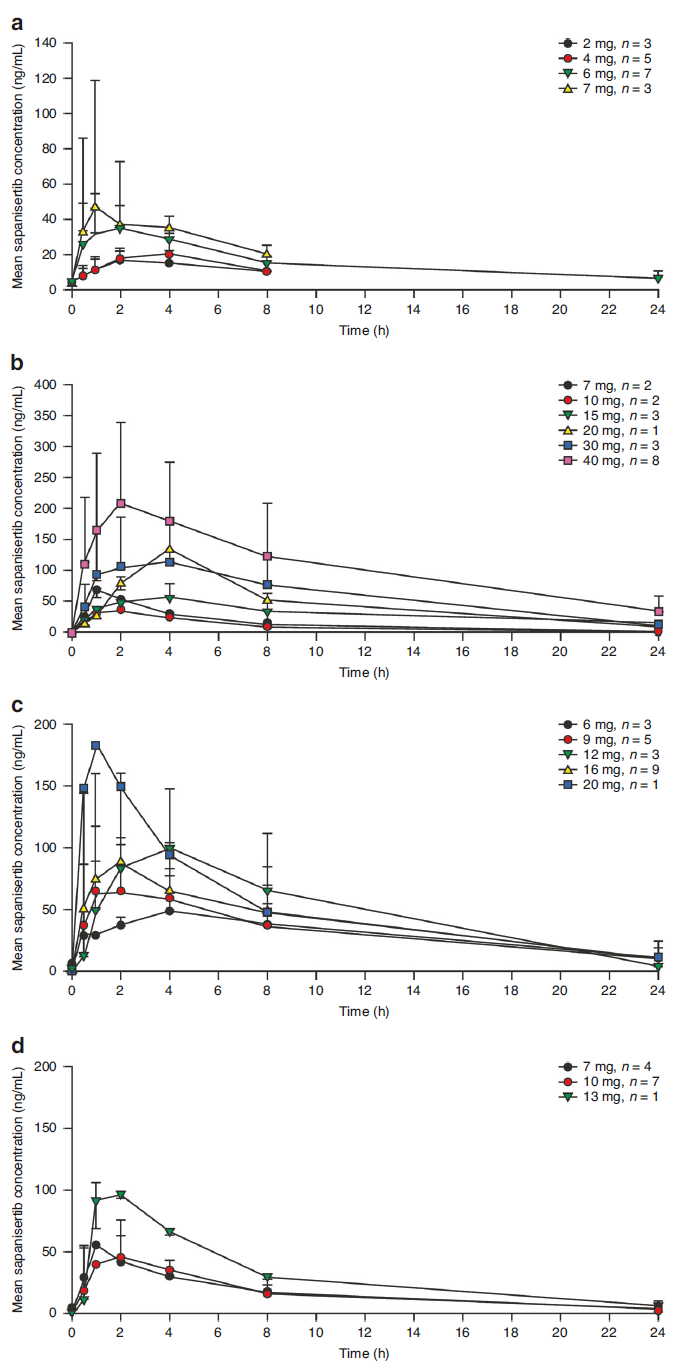
Sapanisertib的药代动力学结果图
结果显示,Sapanisertib的最大耐受剂量为6μmg QD、40μmg QW、9μmg QD×3dQW和7μmg QD×5dQW。常见的剂量限制性毒性(DLTs)包括高血糖症、黄斑丘疹(QD)、乏力和口腔炎(QD×3dQW/QD×5dQW);根据DLT评估的耐受性分析,选择5μmg QD和30μmg QW进行扩展队列的给药研究。一位RCC患者获得完全缓解;9位患者获得部分缓解(其中肾细胞癌患者7位;膀胱癌和子宫内膜癌各1位)。药代动力学显示,Sapanisertib是时间线性的,并支持重复给药。药效学研究结果表明,与治疗相关的TORC1/2生物标志物减少。
综上,在该1期研究中,药物Sapanisertib显示出可控的安全性,且在肾细胞癌和子宫内膜癌中观察到初步的抗肿瘤活性。
原始出处:
Voss, M.H., Gordon, M.S., Mita, M. et al. Phase 1 study of mTORC1/2 inhibitor sapanisertib (TAK-228) in advanced solid tumours, with an expansion phase in renal, endometrial or bladder cancer. Br J Cancer (11 September 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Br J Cancer#点击查看更多相关话题 或评论点击插入您喜欢的话题
68
#SAP#
38
Sapanisertib显示出可控的安全性,且在肾细胞癌和子宫内膜癌中观察到初步的抗肿瘤活性。
96
#APA#
32
#晚期实体瘤#
38
学习
96
了解
98