JAHA:尿路感染患者使用氟喹诺酮类药物治疗与主动脉瘤和主动脉夹层之间的相关性
2022-03-01 MedSci原创 MedSci原创
与第一代或第二代头孢菌素治疗相比,氟喹诺酮类药物与尿路感染患者的主动脉瘤和主动脉夹层风险增加无关。然而,在接受氟喹诺酮类药物治疗的患者中仍然存在显著的死亡风险。
氟喹诺酮类药物是推荐用于治疗复杂性尿路感染的一线抗生素,经常报告发生主动脉瘤和主动脉夹层等不良反应。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员评估了服用氟喹诺酮类药物治疗是否会增加尿路感染患者患主动脉瘤和主动脉夹层的风险。

研究人员使用中国台湾健康保险研究数据库来确定了接受氟喹诺酮类药物和第一代、第二代或第三代头孢菌素等单一抗生素治疗的尿路感染患者。受试者一年内的主动脉瘤和主动脉夹层诊断是本研究的主要观察事件。研究人员采用多Cox回归模型的多变量分析比较了氟喹诺酮类药物与第一代或第二代头孢菌素类药物治疗后的主动脉瘤和主动脉夹层危害风险。研究人员进行了倾向评分匹配以减少由测量的混杂变量引起偏差的可能性。
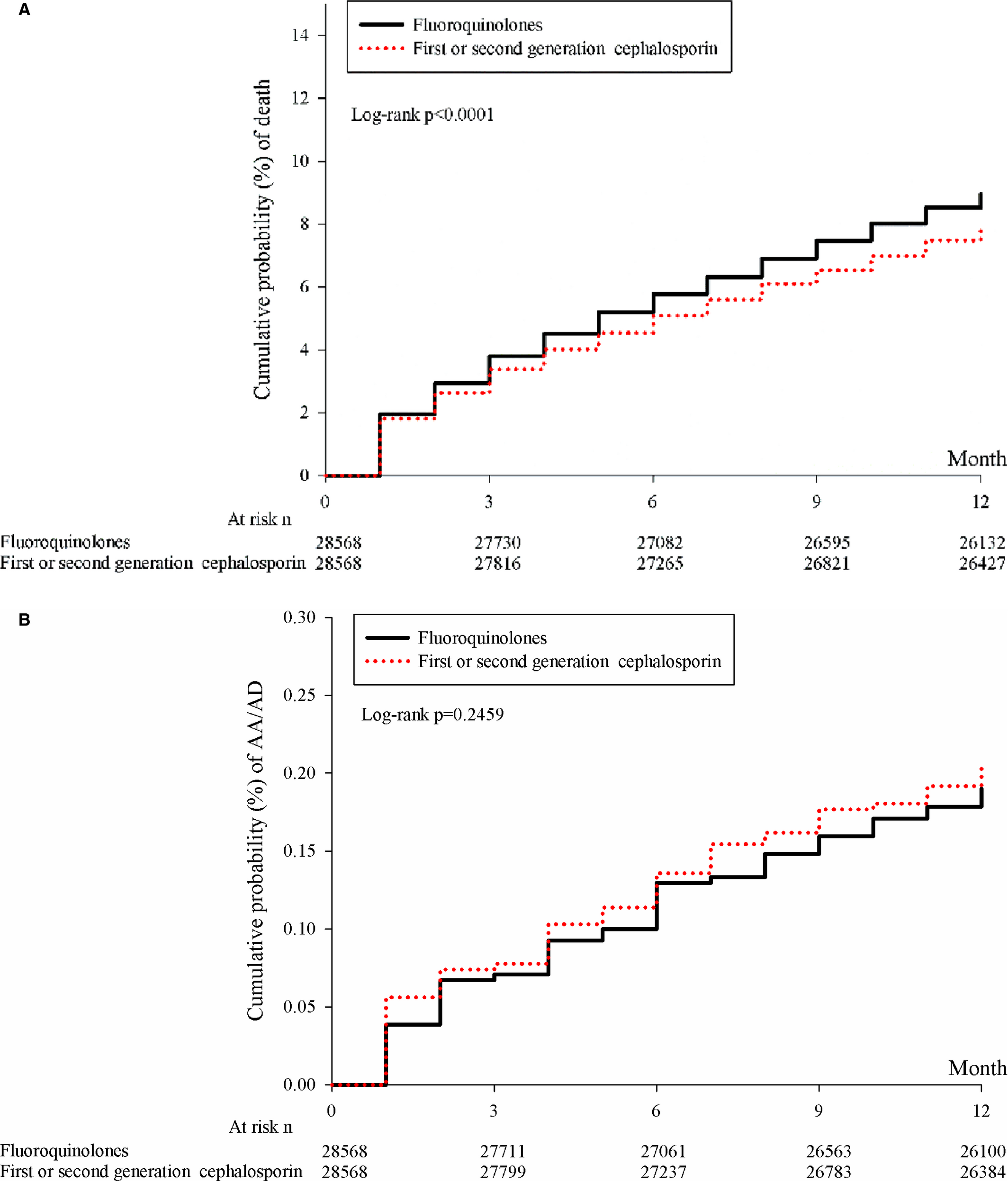
在选择的1249944例尿路感染患者中,通过倾向评分匹配分析后,28568例患者被分配到每个抗生素治疗组中。氟喹诺酮类药物与第一代或第二代头孢菌素类药物的主动脉瘤和主动脉夹层发生率没有显著差异(调整后的HR[aHR]为0.86[95%CI为0.59-1.27])。然而,氟喹诺酮类药物组的死亡率增加(aHR为1.10[95%CI为1.04-1.16])。
由此可见,与第一代或第二代头孢菌素治疗相比,氟喹诺酮类药物与尿路感染患者的主动脉瘤和主动脉夹层风险增加无关。然而,在接受氟喹诺酮类药物治疗的患者中仍然存在显著的死亡风险。考虑到尿路感染患者的主动脉瘤和主动脉夹层风险,当务之急是用足够的抗生素控制感染,而不是排除氟喹诺酮类药物。
原始出处:
Yin‐Yang Chen.et al.Association Between Aortic Aneurysm and Aortic Dissection With Fluoroquinolones Use in Patients With Urinary Tract Infections: A Population‐Based Cohort Study.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.023267
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#氟喹诺酮类药物#
49
#喹诺酮#
50
#相关性#
52
尿路感染
54
#AHA#
45
#主动脉#
34
#主动脉瘤#
0
#动脉夹层#
30
#氟喹诺酮#
39