Cardiovasc Diabetol:甘油三酯葡萄糖指数越高,颈动脉粥样硬化的可能性越大!
2022-03-19 Nebula MedSci原创
TyG指数可能是一种有前途的动脉粥样硬化标志物
卒中(俗称中风)是中国成人死亡和严重残疾的主要原因,其特点是卒中复发率和心血管事件发生率高。动脉粥样硬化是脑卒中发生和复发的主要病理基础。因此,早期识别高危患者并及时控制动脉粥样硬化进展对预防卒中发生至关重要。
胰岛素抵抗 (IR) 是众所周知的多种心血管疾病(CAD)的预测因子。虽然高胰岛素-正常血糖是评估胰岛素抵抗的金标准,但由于检测过程复杂和经济原因,在临床环境中并不适用。因此,我们迫切需要一种简单、稳定、易于实施的胰岛素抵抗标志物。
甘油三酯葡萄糖 (TyG) 指数已被发现与心血管事件发生和复发风险增加有关,动脉粥样硬化是主要的推测机制。但是,目前关于TyG指数与动脉粥样硬化之间关系的数据,特别是在缺血性卒中的情况下,还很少。本研究旨在探讨TyG指数与缺血性卒中患者颈动脉粥样硬化之间的相关性。
共招募了1523位有TyR指数和颈动脉成像数据的缺血性卒中患者。TyG指数=In[空腹甘油三酯(mg/dL) x 空腹血糖(mg/dL)/2]。根据颈总动脉内膜中层厚度(cIMT)评估颈动脉粥样硬化,异常cIMT定义:平均cIMT和最大cIMT值≥1mm。最后采用多变量逻辑回归模型和限制三次样条模型评估TyG指数与异常cIMT之间的相关性。
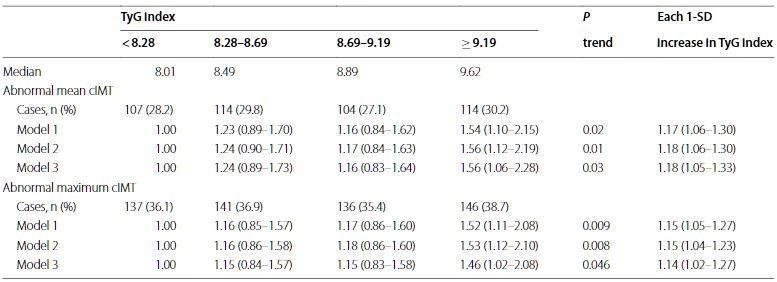
根据TyG指数分组的异常cTMI的优势比
根据TyG指数将患者分成4组(Q1-Q4),与Q1组相比,Q4组平均cIMT异常的优势比(OR)为1.56,最大cIMT异常的OR为1.46。TyG指数和异常平均cIMT及异常最大cIMT之间均存在线性相关性(p分别是0.005和0.027)。此外,TyG指数还提供了超出既定风险因素的增量预测能力,表现为净重新分类改进和综合区分改进的增加(所有p<0.05)。
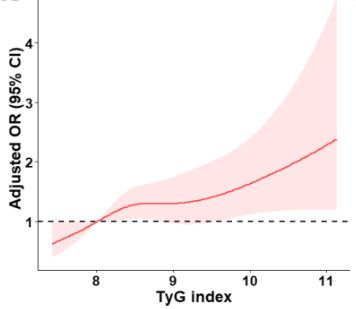
TyG指数与卒中患者颈总动脉内膜中层厚度的相关性
综上,TyG指数越高,缺血性卒中患者越可能存在颈动脉粥样硬化,提示TyG指数可能是一种有前途的动脉粥样硬化标志物。
原始出处:
Miao, M., Zhou, G., Bao, A. et al. Triglyceride-glucose index and common carotid artery intima-media thickness in patients with ischemic stroke. Cardiovasc Diabetol 21, 43 (2022). https://doi.org/10.1186/s12933-022-01472-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#ASC#
43
#粥样硬化#
57
#DIA#
47
#BET#
43
#颈动脉#
44
#颈动脉粥样硬化#
44
学到了
62