Eur Heart J:主动脉直径与心血管风险相关?
2021-07-22 “ Clinic門诊新视野”公众号 “ Clinic門诊新视野”公众号
在传统腹主动脉瘤(AAA)筛查中,主动脉直径可能在评估心血管风险方面发挥作用。但是,对于不患AAA但是心血管风险管理欠佳的人群,主动脉直径的评估没有得到充分的利用。近期,Sidloff等[1]通过回顾
在传统腹主动脉瘤(AAA)筛查中,主动脉直径可能在评估心血管风险方面发挥作用。但是,对于不患AAA但是心血管风险管理欠佳的人群,主动脉直径的评估没有得到充分的利用。近期,Sidloff等[1]通过回顾性分析3个数据库,研究了主动脉直径与未来心血管风险的关联,并将其发表于European Journal of Vascular and Endovascular Surgery。
研究目的
探讨主动脉直径与未来心血管风险之间的关联。
研究方法
回顾性分析筛查动脉瘤疾病的3个男性参与者数据库。影像和临床资料来自三个独立来源:
1)多中心动脉瘤筛查研究(MASS)的男性列队(n = 26,882);
2)2013~2014年英国NHS AAA筛查计划(NAAASP)的男性队列研究(n=237,441)与NHS住院和死亡登记数据相关;
3)弗雷明汉心脏研究(FHS)后代队列(n=649,男性)。通过超声或CT扫描测量的最大主动脉直径与心血管预后之间的相关性。
研究结果
MASS研究队列:共1,336名(4.9%)AAA患者,平均主动脉直径为3.8±1.2 cm(未患病患者数据未测)。随访13年,相较于未患AAA患者,AAA患者的心血管死亡率更高(13.4% vs. 24.3%,P<0.001)。此外,AAA患者的非心血管死亡率也更高(36.2% vs. 23.6%,HR 1.86,95% CI 1.69-2.06),并且就年龄调整后,这种相关性依然存在(表1)。
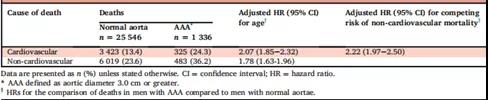
表1. MASS研究中正常主动脉和AAA患者心血管死亡率和非心血管死亡率数据比较
NAAASP队列:主动脉直径为2.5~2.9 cm男性人群的心血管死亡风险显着高于正常主动脉直径人群(0.96% vs. 0.36%,HR 2.63,95% CI 1.84-3.76),在AAA患者中这一风险进一步增加(HR 2.91,95% CI 2.00-4.25)(表2);此外,主动脉直径临界值不同导致死亡的主要原因也有所不同,正常尺寸人群为恶性肿瘤,直径为2.5~2.9 cm和AAA患者均为心血管原因(图1)。进一分析还发现,主动脉直径过小(0.49~1.24 cm)同样会增加心血管死亡风险(HR 3.04,95% CI 1.77-5.21)。这一结果表明主动脉直径和心血管死亡风险之间存在U型关联。
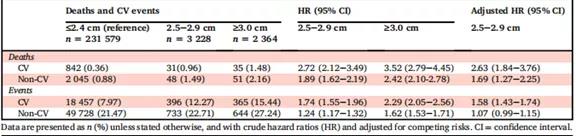
表2. NAAASP队列中主动脉直径增加,主要不良心血管事件和死亡风险增加

图1. NAAASP队列中主动脉直径不同主要死亡原因也不同
FHS列队:平均随访12.3年。有23例个体描述了准确的死亡原因,其中20例(87%)死因与心血管相关。进一分析可知,主动脉直径≥2.5 cm(HR 1.88,95% CI 1.03-3.44,P<0.001)和年龄(AOR 1.06,95% CI 1.04-1.09,P<0.001)与未来主要心血管事件发生风险显着相关。
结 果
不管是否诊断为AAA,在参加AAA筛查的男性人群中,异常主动脉直径和未来心血管事件的发生率和死亡率相关。这些数据的利用有可能改善心血管风险的预防管理。
原始出处:
Sidloff DA, Saratzis A, Thompson J, et al. Infra-Renal Aortic Diameter and Cardiovascular Risk: Making Better Use of Abdominal Aortic Aneurysm Screening Outcomes. Eur J Vasc Endovasc Surg. 2021; https://doi.org/10.1016/j.ejvs.2021.03.013.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#血管风险#
40
#ART#
41
#主动脉#
41
#HEART#
39