Circulation:经手术与经导管主动脉瓣置换术术后1年的心超检查对比
2020-05-23 QQY MedSci原创
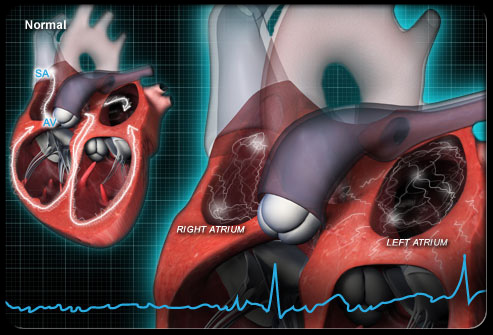
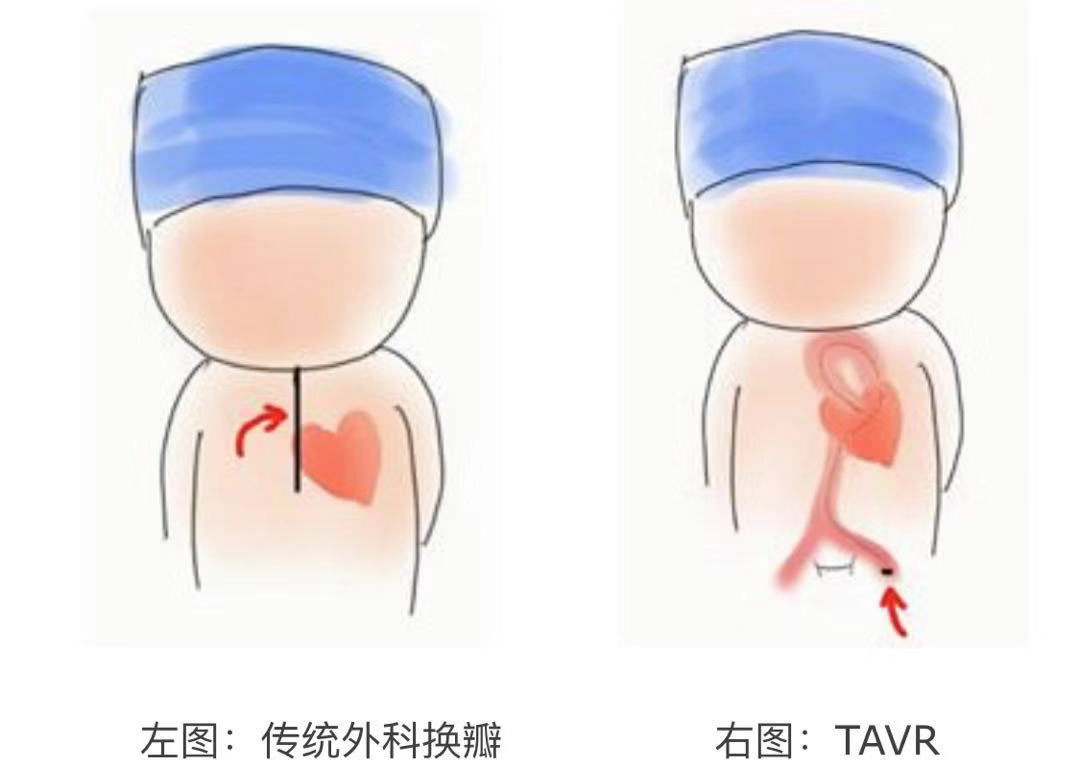
本研究旨在比较低风险的重度主动脉狭窄患者经手术主动脉瓣置换术(SAVR)或经导管主动脉瓣置换术(TAVR)后的超声心动图表现。
PARTNER 3试验将1000位低风险的重度主动脉瓣狭窄患者随机分至SAVR组或经股TAVR(置换可膨胀的3瓣SAPIEN)。由2个超声心动图核心实验室组成的联合研究小组分析了患者在基线、术后30天和术后1年时的经胸超声心动图。
在30天内,TAVR组和SAVR组中度或重度主动脉返流(AR)的百分比均较低,无统计学差异(0.8% vs 0.2%,p=0.38).30天内,TAVR治疗后的患者的轻度AR比SAVR治疗后的更常见(28.8% vs 4.2%,p<0.001)。1年时,AVR组和SAVR组的平均跨瓣梯度和主动脉瓣面积相近(13.7±5.6 vs 11.6±5.0 mmHg,p=0.12;1.72±0.37 vs 1.76±0.42 cm2,p=0.12)。30天时,两组重度假体-患者不匹配的比例较低且相近(4.6% vs 6.3%,p=0.30)。
TAVR组反映左心室总血流动力学负荷的瓣膜动脉阻抗(Zva)低于SAVR组(3.7±0.8 vs 3.9±0.9 mmHg/mL/m2; p<0.001)。与基线相比,1年时SAVR组的三尖瓣环面收缩偏移减小、中重度三尖瓣反流的百分比增加,而TAVR组的保持不变。无论哪个治疗臂,高Zva和低三尖瓣环面收缩期偏移都与1年时死亡、中风和再次住院的综合终点风险增加有关,但中重度AR或重度假体-患者错配与其无关。
对于低手术风险的重度主动脉瓣狭窄患者,采用3瓣SAPIEN的TAVR治疗的中重度AR发生率与采用SAVR的相似,但轻度AR的发生率较SAVR的更高。TAVR和SAVR治疗的跨瓣梯度、瓣膜面积、严重假体-患者失配的百分比以及左心室质量恢复均相似。SAVR与术后1年时的右心室收缩功能明显恶化和更严重的三尖瓣反流相关。高Zva和低三尖瓣环面收缩期偏移均与术后1年时的预后不良相关,而AR和重度假体-患者错配与其无关。
原始出处:
Philippe Pibarot,et al. Echocardiographic Results of Transcatheter Versus Surgical Aortic Valve Replacement in Low-Risk Patients.Circulation. 2020;141:1527–1537
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#置换#
37
#主动脉瓣#
32
#主动脉瓣置换术#
47
#主动脉#
40
#经导管#
35
#经导管主动脉瓣置换#
31
#置换术#
29