J Invest Dermatol:口服富马酸二甲酯在咪喹莫特小鼠模型中靶向HCA2表达的研究
2022-03-07 医路坦克 MedSci原创
口服富马酸二甲酯(DMF)在欧洲国家被广泛用于系统治疗银屑病,本研究的目的是在银屑病样皮炎的小鼠Imiquimod(Imq)模型中研究DMF治疗HCA2的细胞靶点。
口服富马酸二甲酯(DMF)在欧洲国家被广泛用于系统治疗银屑病,在世界范围内被广泛用于多发性硬化症(MS)。DMF在体内迅速水解为富马酸单甲酯,口服给药后在患者或健康人的血液中检测不到DM。尽管进行了广泛的研究,但口服DMF治疗的明确作用模式尚未完全阐明。
以前的研究已经强调了细胞氧化还原调节在DMF治疗MS的神经保护效应中的作用,特别是血红素加氧酶1(HO-1)的诱导和核因子(红系衍生的2)样2(Nrf2)途径的激活。然而,我们也知道MMF是羟基羧酸受体2(HCA2)的激动剂。鉴于多种表达HCA2的细胞类型(即角质形成细胞、朗格汉斯细胞(LCS)和中性粒细胞)参与了银屑病的发病机制,本研究的目的是在银屑病样皮炎的小鼠Imiquimod(Imq)模型中研究DMF治疗HCA2的细胞靶点。
为探讨二甲基甲酰胺(DMF)对IMQ模型保护作用中对Hca2的需求,对Hca2+/+和Hca2-/-小鼠进行口服DMF或溶剂预处理7d后,将Aldara®应用于所有小鼠的背部,连续5d,观察Hca2+/+和Hca2-/-小鼠Hca2+/+和Hca2-/-的保护作用。与使用Aldara®的车辆注射Hca2+/+小鼠相比,DMF处理的Hca2+/+小鼠显示出较少的鳞屑和皮损发红(图S1b),表皮厚度减少了39%(图1a+b)。这一效应在Hca2-/-小鼠中被取消。这些结果表明,DMF减轻了ImQ引起的皮肤炎症的严重程度,HCA2是这种保护作用所必需的。
图1:DMF治疗以HCA2依赖的方式减少表皮厚度。
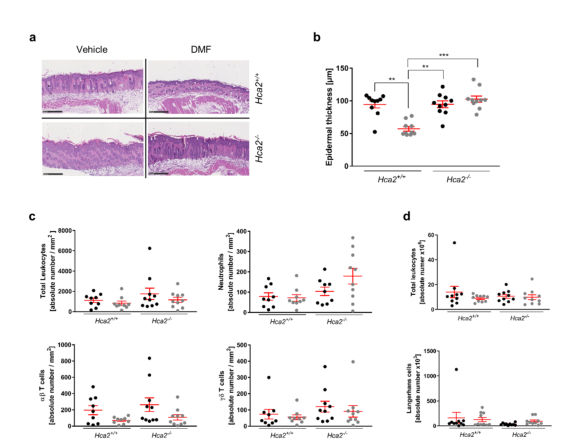
(A)有代表性的第13天小鼠背部皮肤的HE切片。标尺=500µm。(B)表皮厚度的定量。(C)取背部皮肤组织,酶消化,计数免疫细胞,免疫组化检测CD45、αβ-TcR、Ly6G和γδ-TcR,以确定细胞群的特征。(3)取背部皮肤活检组织,计数免疫细胞并进行CD45TcR、TcR、LY6G和TcR免疫染色。(D)机械破碎实验小鼠的SDLN,计数获得的细胞,进行CD45、MHCII和CD207免疫组化染色,流式细胞仪分析。黑色=车辆,灰色=DMF。取值为均值±扫描电镜(n=10只/组)。多项比较经方差分析(b和d)及邓尼特校正,*p<0.001;**p<0.01;*p<0.001。
图2:角质形成细胞是口服DMF保护作用的潜在靶点。
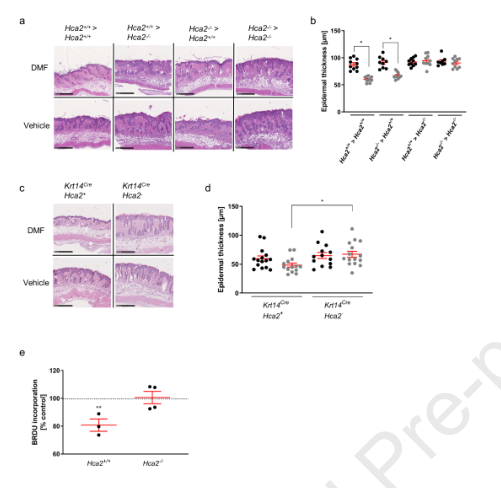
(A)经Aldara®处理的嵌合体背部皮肤的代表性H&E染色切片。刻度尺=500µm。(B)表皮厚度的量化。黑点=车辆,灰点=DMF。取值为均值+扫描电镜(n=10只/组)。(C)经Aldara®处理的Krt14Cre-Hca2+(Hca2表达)和Krt14Cre-Hca2-(角质形成细胞特异性Hca2基因敲除)动物背部皮肤的代表性H+E切片。比例尺=500µm。(D)汇总了15只小鼠/组的表皮厚度数据。黑色=车辆,灰色=DMF。(E)分离新生小鼠角质形成细胞,以100µM MMF或PBS培养为对照。用BrdU掺入法检测细胞增殖情况。增殖以相对对照组百分比计算(n=3~5)。水平线表示均值±扫描电镜。统计学分析采用Kruskal-Wallis检验(b和d)加Dunnett多重比较校正或方差分析(E)加Tukey多重比较检验,*p<0.05,**p<0.01。
HCA2在口服DMF消除皮肤炎症中的关键作用与之前的研究结果相似,该结果表明口服DMF对实验性自身免疫性脑脊髓炎(EAE)(MS的小鼠模型)和大疱性获得性大疱性表皮松解症(EBA)(类天疱疮皮肤病的模型)的保护作用是必不可少的。在这两种疾病中,中性粒细胞被认为是DMF治疗的主要目标。研究表明,在银屑病患者中,DMF治疗可以减少外周中性粒细胞的数量。因此,我们假设口服DMF在IMQ模型中通过HCA2依赖的方式调节中性粒细胞。因此,我们调查了在使用Aldara®时,DMF处理是否改变了皮肤免疫细胞的浸润。DMF治疗后CD45+白细胞总数无明显变化。口服DMF后,皮肤中性粒细胞或HCA2--T细胞亚群的数量没有明显变化(图1c)。这些数据表明,DMF治疗并不能通过减少中性粒细胞(或其他免疫细胞)在皮肤中的募集来预防皮肤炎症。
因此,一个潜在的作用机制是口服DMF在体内产生MMF,最初通过角质形成细胞上的HCA2发出信号,导致IMQ暴露后细胞过度增殖减少,趋化因子和AMP表达减少。由于短期ImQ模型代表急性银屑病样炎症,在这种情况下口服DMF的角质形成细胞特异性效应可能转化为抑制银屑病患者的皮损进展。有趣的是,DMF治疗在NRF2-/-和NRF2+/+小鼠中对ImQ引起的皮肤炎症有相似程度的改善。这一结果表明,NRF2通路不是DMF皮肤保护所必需的。
总而言之,这里显示的数据提供了明确的证据,表明口服DMF通过HCA2依赖的方式保护皮肤免受炎症。具体地说,携带HCA2的角质形成细胞而不是血液免疫细胞似乎是DMF治疗的早期关键靶点。这些结果不排除在银屑病治疗中存在额外的HCA2依赖和独立现象。然而,对角质形成细胞HCA2信号在DMF治疗效果中的重要性的认识表明,更精确地靶向这一途径可能会改善银屑病患者的临床结果。
文献来源:Suhrkamp I, Morrison PJ, Assmann JC,ORAL DIMETHYL FUMARATE TARGETS HCA-EXPRESSING SKIN CELLS IN THE IMIQUIMOD MOUSE MODEL.J Invest Dermatol 2022 Feb 18;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#EST#
29
#HCA#
38
#小鼠模型#
57
#富马酸二甲酯#
33
#CA2#
45