Blood:镰刀细胞性贫血患儿的沉默性脑梗死发生在脑血流低的边界区域
2018-10-24 MedSci MedSci原创
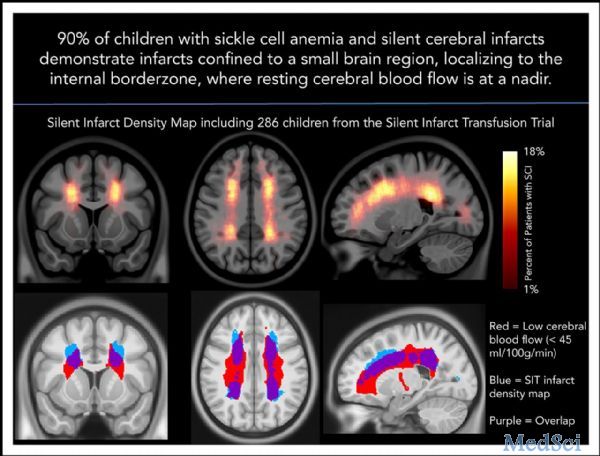
中心点:SCI密度图揭示了额叶和顶叶深层白质中主要的SCI位置。SCI密度峰值出现在脑血流量最低的脑区。摘要:沉默性脑梗死(SCIs)与镰刀细胞性贫血(SCA)的认知障碍相关。SCI风险因素包括低血红蛋白和收缩压升高;但是,其发生发展的机制尚不明确。Andria L. Ford等人开展一前瞻性研究,评估SCA患儿的SCIs,明确SCI密度增大的脑区。研究人员对“在脑血流最低的区域梗死密度最大,进一
中心点:
SCI密度图揭示了额叶和顶叶深层白质中主要的SCI位置。
SCI密度峰值出现在脑血流量最低的脑区。
摘要:
沉默性脑梗死(SCIs)与镰刀细胞性贫血(SCA)的认知障碍相关。SCI风险因素包括低血红蛋白和收缩压升高;但是,其发生发展的机制尚不明确。Andria L. Ford等人开展一前瞻性研究,评估SCA患儿的SCIs,明确SCI密度增大的脑区。研究人员对“在脑血流最低的区域梗死密度最大,进一步限制了慢性贫血时的大脑氧供应”这一假设进行验证。
在包含286位儿童的沉默性梗死输血(SIT)试验中,神经放射学和神经病学委员会达成共识。绘制每一个梗死的轮廓,并对应到脑图上,以创建梗死密度图。为评估脑血流作为梗死密度的功能,研究人员在一个独立的儿科SCA队列中进行了伪连续动脉自旋标记。将血流图与SIT试验的梗死密度图相对应。对比SIT试验中低、中、高梗死密度脑区的平均血流。用Logistic回归曲线评估临床随访3年中发生的显性卒中的临床和影像学预测因素。
SIT试验梗死密度图表明在额叶和顶叶的深层白质中,SCI密度增加。一个相对较小的区域,占脑容积的5.6%,涵盖了90%的儿童SCIs。在梗死密度最大的脑区,脑血流最低(p<0.001)。起始梗死体积和网织红细胞计数可预测显性卒中。在儿科SCA中,SCIs对称的位于脑血流最小的深层白质中。
原始出处:
Andria L. Ford,et al. Silent infarcts in sickle cell disease occur in the border zone region and are associated with low cerebral blood flow. Blood 2018 132:1714-1723; doi: https://doi.org/10.1182/blood-2018-04-841247
本文系梅斯医学(MedSci)原创编译,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#脑血流#
35
#细胞性#
29
#脑梗#
21