Behavioural Brain Research:安全信号的神经生理学反应和心脏迷走神经控制的作用
2020-09-28 MedSci原创 MedSci原创
在恐惧相关障碍(如创伤后应激障碍(PTSD)、恐惧症)中,安全信号学习的缺陷是很明显的。目前的研究使用恐惧条件反射范式来测试眨眼惊吓和事件相关脑电位(ERP)潜伏期安全信号学习措施之间的关联,以及心脏
在恐惧相关障碍(如创伤后应激障碍(PTSD)、恐惧症)中,安全信号学习的缺陷是很明显的。目前的研究使用恐惧条件反射范式来测试眨眼惊吓和事件相关脑电位(ERP)潜伏期安全信号学习措施之间的关联,以及心脏迷走神经控制(安全学习所需的自上而下抑制措施)的作用。创伤后应激障碍(PTSD)患者可能无法抑制他们的恐惧反应,尽管缺乏威胁,但他们可能会经历长时间的觉醒和恐惧。同样,惊恐障碍患者在抑制对非危险的身体感觉和相互感知线索的恐惧能力方面存在缺陷(例如,在运动中心跳加快),而那些患有恐惧症的人在一系列非危险物体或情况下。对这些人群的研究表明,不良的安全信号学习是恐惧相关疾病的一种特殊表型,它将他们与健康人群区分开来。
方法:参与者为49名年龄在17至28岁之间的创伤暴露妇女。对条件刺激相关(CS+)和不相关(CS-)的条件刺激和厌恶性非条件刺激的眼球震颤反应和ERP振幅/潜伏期进行了推导。ERPs包括P100和晚期正电位(LPP),分别反映早期视觉加工和持续的情绪编码。用静息心率变异性(HRV)评价心脏迷走神经控制。脑电图数据用BrainVision Analyzer 2.04软件(Brain Products,德国)处理,并参考平均参考值,使用离线滤波器(0.1-30 Hz)。采用独立成分分析(ICA)识别和去除眼球运动和眼球环伪影。每个EEG和EOG通道由单独的EEG100C和EOG100C模块(Biopac MP100C系统,Biopac Systems,Goleta,CA)用模拟带通滤波器从0.1到35 Hz进行放大。在频率为1khz/s的情况下,对EEG样本进行采样(频率为1khz/s)。使用AcqKnowledge 3.8.1为Biopac MP100C系统收集脑电图和EOG数据。
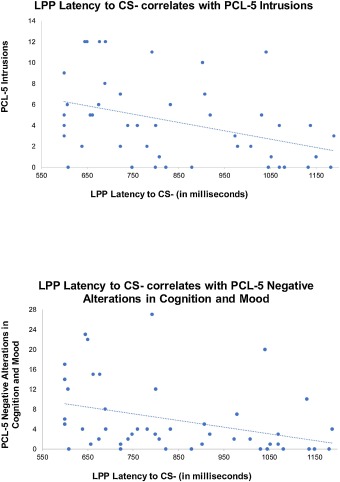
结果:P100和LPP潜伏期CS-(安全信号刺激)与惊吓显著负相关,但与CS+无关。LPP-CS-潜伏期与创伤后应激障碍评分呈显著负相关,这种关系被迷走神经控制所调节,因此这种影响只存在于HRV较低的人群中。
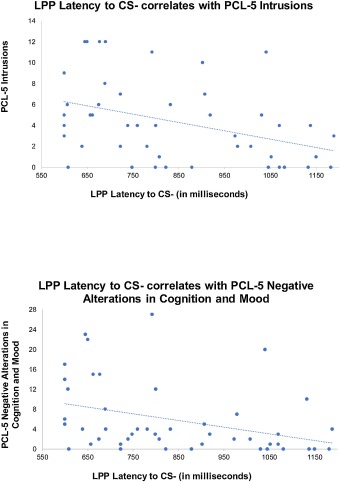
结论:基于ERP的安全信号学习标记物与CS-(但不是CS+)和PTSD症状的惊吓反应相关,表明这些标记物可能与恐惧相关的疾病相关。以心率变异性为指标的心脏迷走神经控制是这些联系的调节因素,可能与安全信号学习有关。
Seligowski, A.V., et al., Neurophysiological responses to safety signals and the role of cardiac vagal control. Behavioural Brain Research, 2021. 396: p. 112914.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#生理学#
54
#HAV#
39
#神经控制#
44
#神经生理#
45
考虑到非标准化的疾病标准,应考虑进一步设计良好的前瞻性试验以证实这些结果。
86
#EHA#
39
#Research#
26
学习了
101
#学习#学习了
98
很好的学习了!
96