硬膜外麻醉致导管椎管内断裂一例
2019-03-26 李洋 魏智彬 云利兵 临床误诊误治
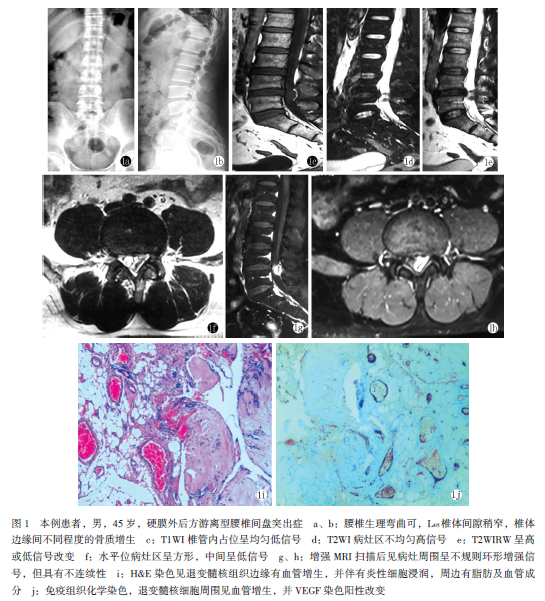
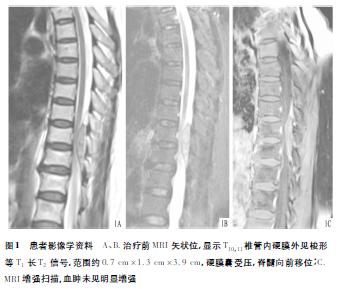
女,43岁。因急性阑尾炎入甲医院,拟急诊行持续硬膜外麻醉阑尾切除术。术前检查脊柱及四肢无畸形,活动自如,腰椎无压痛。术中患者取右侧屈膝位,穿刺点为胸11~12,常规消毒、铺巾后经旁路穿刺,到达硬膜外腔后向上置管,退出穿刺针调整硬膜外置管过程中导管突然断裂,遂急诊切开皮肤约3 cm,组织钳依次钝性分离皮下组织,寻找硬膜外导管残端未果,立即请邻近上级医院麻醉科会诊,亦未找到硬膜外导管残端,后缝合切口。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#椎管内#
37
#椎管#
30
#硬膜外#
33
#硬膜外麻醉#
29
学习了谢谢分享
76