Neurology:脑卒中发病后15-180天添加西洛他唑联合阿司匹林/氯吡格雷双重抗板治疗降低缺血性卒中复发风险
2022-02-09 Naomi MedSci原创
近日,有研究人员通过分析来自 csps 网站的数据对假设进行检验。研究发现,对于急性非心源性栓塞性卒中患者,服用阿司匹林或氯吡格雷,在卒中发病后15至180天添加西洛他唑可降低复发性缺血性卒中的风险。
尽管与单一使用阿司匹林相比,阿司匹林联合氯吡格雷(ASA+CLO)的双重抗血小板治疗(DAPT),能够降低轻度缺血性卒中、高危短暂性脑缺血发作(TIA)后早期复发的风险,但在首月应用后,由于比单一使用阿司匹林有更高的大出血风险,其降低卒中风险的作用会减弱。
荟萃分析表明,ASA+CLO的DAPT主要在卒中发病后24小时内开始,在卒中发病后3个月内可显著降低缺血性卒中再发的风险,但在卒中发病后1月内显著增加大出血的风险。在卒中发生30天内早期启动DAPT并使用替卡格雷洛和阿司匹林,与单用阿司匹林相比,已被证明可降低卒中或死亡的复合风险,但这种组合增加严重出血风险。此外,2月后的影响尚未被探讨。
西洛他唑是一种磷酸二酯酶3抑制剂,西洛他唑联合阿司匹林(CLZ+ASA)或西洛他唑联合氯吡格雷(CLZ+ CLO)可以降低复发性缺血性卒中的风险。在西洛他唑联合抗血小板药物预防脑卒中的对照试验中,与单独使用阿司匹林或氯吡格雷相比,长期使用中位数为1.4年的西洛他唑联合阿司匹林或氯吡格雷可以降低复发性缺血性卒中的高风险患者的严重出血风险。如果西洛他唑在卒中后一个月内开始使用有效,则可以通过将阿司匹林或氯吡格雷改用西洛他唑,并在卒中后多年持续使用西洛他唑来获得有希望的治疗策略。
近日,有研究人员通过分析来自 csps 网站的数据对假设进行检验,即在最初几周内开始使用西洛他唑,与单独使用阿司匹林或氯吡格雷相比,是否更有效、更安全。其主要研究问题是确定最佳启动时间西洛他唑联合阿司匹林或氯吡格雷治疗高危非心源性缺血性卒中。
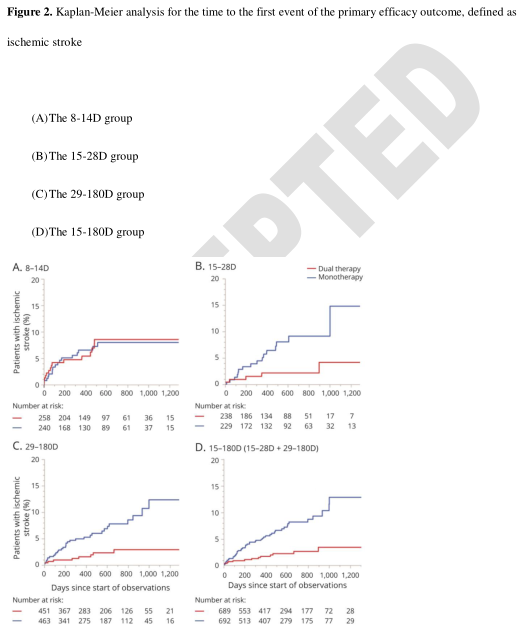
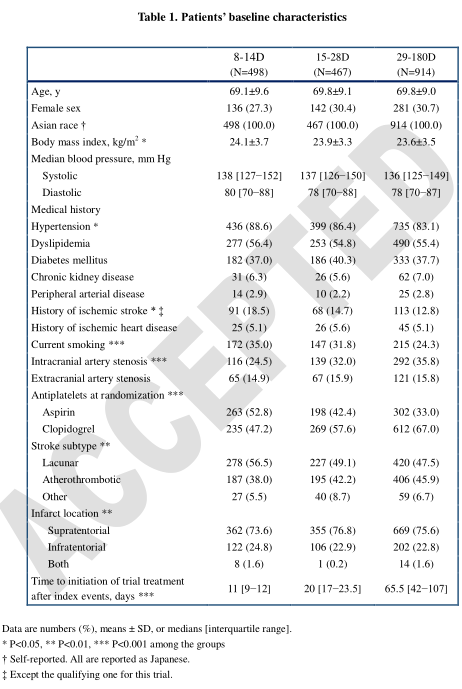
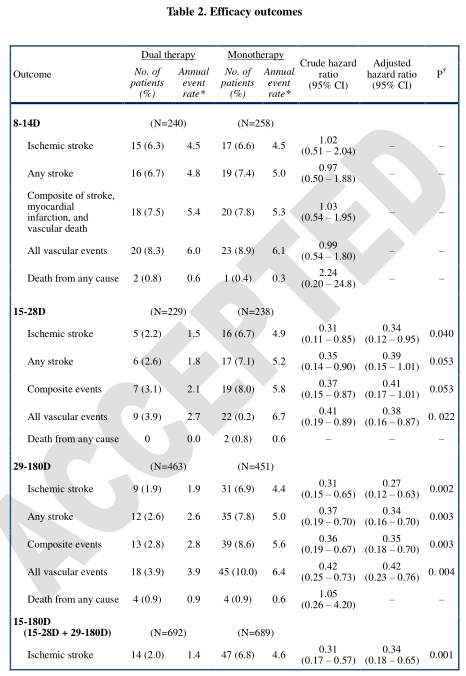
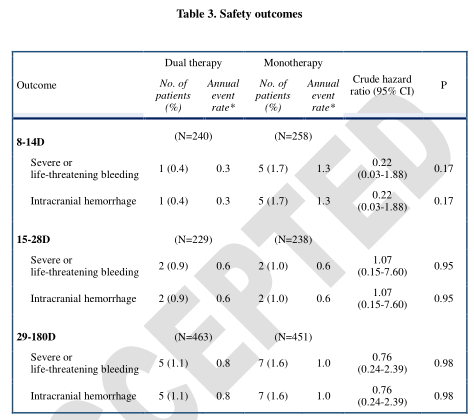
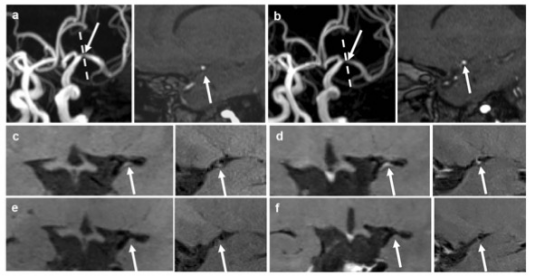
在这项随机对照试验的分析中,在卒中发病后8-180天之间的患者被随机分配单独服用阿司匹林或氯吡格雷,或者西洛他唑与阿司匹林或氯吡格雷联合服用。根据试验治疗的开始时间分为3组: 发病后8-14d 开始治疗组(8-14d 组) ,发病后15-28d 开始治疗组(15-28d 组) ,29-180d 开始治疗组(29-180d 组)。主要疗效结果是缺血性卒中的首次复发。安全结果包括严重或危及生命的出血。
- 1879例患者中,8-14d 组498例,15-28d 组467例,29-180d 组914例。
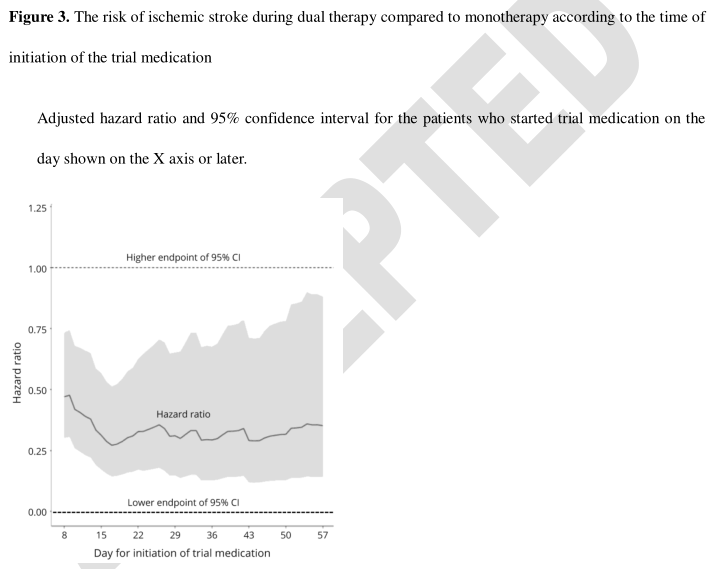
- 对于缺血性卒中的复发,在试验治疗组和三分法治疗组之间存在显著的逐组治疗相互作用。缺血性脑卒中双重治疗组复发率低于单一治疗组(年化率分别为1.5% 和4.9% ,校正危险比为0.34,95% ci 为0.12-0.95)和29-180d 组(分别为1.9% 和4.4% ,0.27,0.12-0.63) ,8-14d 组复发率相似(两者均为4.5% ,1.02,0.51-2.04)。
- 双重治疗组与单一治疗组出现严重或危及生命的出血情况相似(粗危险比为0.22,95% CI 为0.03-1.88,8-14d,1.07,0.15-7.60,29-180d 组为0.76,0.24-2.39)。
长期双重抗血小板治疗使用西洛他唑在卒中发病后15-180天开始,比治疗开始后8-14天,更有效的二次卒中预防比单一治疗不增加出血风险。
这项研究提供了 ii 类证据,对于急性非心源性栓塞性卒中患者,服用阿司匹林或氯吡格雷,在脑卒中发病后15至180天添加西洛他唑可降低复发性缺血性卒中的风险。
文献来源:Toyoda, Kazunori et al. “Association of Timing for Starting Dual Antiplatelet Treatment With Cilostazol and Recurrent Stroke: A CSPS.com Trial Post Hoc Analysis.” Neurology, 10.1212/WNL.0000000000200064. 24 Jan. 2022, doi:10.1212/WNL.0000000000200064
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#Neurol#
48
#缺血性#
51
学习学习
42
#缺血性卒#
37
#复发风险#
48
学习学习
41
学习 学习
54
好文章、学习
50
好
68
学习
66