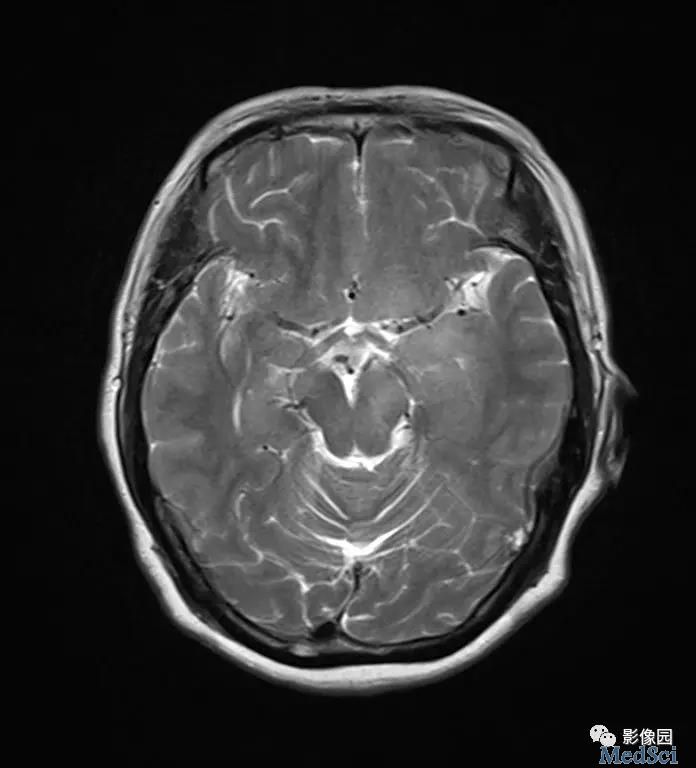
Radiology:DTI和PWI放射组学与高通量测序技术指导IDH野生型胶质母细胞瘤的预后
2020-04-18 shaosai MedSci原创
高通量测序技术(NGS)对肿瘤基因组学分析具有高度敏感性,但其对基于影像学预测指导的临床治疗决策的临床意义较为受限。
背景
高通量测序技术(NGS)对肿瘤基因组学分析具有高度敏感性,但其对基于影像学预测指导的临床治疗决策的临床意义较为受限。
目的
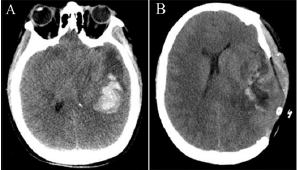
本研究旨在利用扩散加权成像(DTI)和灌注加权成像(PWI)放射组学特征和NGS来预测IDH野生型胶质母细胞瘤的核心信号通路。
材料与方法
利用行NGS和解剖结构性、扩散加权和PWI的患者来建立放射基因组学模型。为了验证预测核心信号通路的模型效能,对IDH 野生型胶质瘤患者进行评价。利用T检验、最小绝对收缩、选择算子法和随机森林法来进行放射基因组学特征选择。利用ROC曲线下面积(AUC)联合放射基因组学特征、年龄、位置、RTK、P53和视网膜母细胞瘤1通路进行评价。
结果
本研究共纳入了120例患者进行评价。其中85例患者为训练组,35例IDH野生型胶质瘤患者为验证组。放射基因学模型共纳入了71个RTK特征、17个P53特征、35个视神经母细胞瘤通道特征。联合模型在RTK(P = .03)、视神经母细胞瘤(P = .03)和基于PWI的P53通道特征(P = .04)要优于基于解剖学成像的结果。联合模型预测核心信号通道RTK、P53和视神经母细胞瘤的AUC值分别为0.88 (95% CI: 0.74, 1) 、0.76 (95% CI: 0.59, 0.92) 、0.81 (95% CI: 0.64, 0.97)。
结论
扩散加权成像和灌注加权成像的放射组学特征模型有助于评价核心信号通路特点,这将能指导IDH野生型胶质母细胞瘤的针对性治疗。
原始出处:
Park JE, Kim HS, Park SY.et al. Prediction of Core Signaling Pathway by Using Diffusion- and Perfusion-based MRI Radiomics and Next-generation Sequencing in Isocitrate Dehydrogenase Wild-type Glioblastoma. DOI: 10.1148/radiol.2019190913
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PWI#
41
#野生型#
40
#胶质母细胞#
37
学习
76
#高通量#
44
#母细胞瘤#
28
#DTI#
47
#高通量测序#
45
#细胞瘤#
28